Orthopedic Surgery deals with diseases and injuries of the locomotive organs, such as bones, joints, ligaments, muscles, tendons, and nerves, which are necessary to support and move the body. Therefore, Orthopedic Surgery covers a wide range of areas including the spine/spinal cord, pelvis, upper extremities (shoulders, elbows, hands, fingers) and lower extremities (crotch, knees, feet, toes). If the locomotor system deteriorates, daily activities will be impaired, and work, going out, sports, traveling, etc. will also be affected. Therefore, keeping the locomotor system healthy leads to a life worth living. Orthopedic Surgery is a specialized department that elucidates the pathology of musculoskeletal diseases and injuries, develops treatment methods, and provides medical care. According to the Basic Survey of Living Conditions conducted by the Ministry of Health, Labor and ministry of Health, Labor and Welfare notation, complaints related to locomotive organs such as low back pain, stiff shoulders, and knee pain are overwhelmingly high, and the role of Orthopedic Surgery, which is the core of locomotive medicine, is becoming more and more important.
Musculoskeletal diseases have various causes such as degeneration, inflammation, trauma, and tumors, and are characterized by a wide range of age groups. In Japan, where the aging of the population has progressed, osteoarthritis and spinal diseases due to degenerative degeneration are on the rise. Due to the growing interest in sports, the number of people participating in various sports is increasing, and sports injuries and disorders are on the rise regardless of age or gender. Injuries to the locomotor system also occur due to occupational accidents and traffic accidents.
Orthopedic Surgery surgery, we perform surgery, conservative therapy such as pain control, and rehabilitation to restore the function of the impaired locomotor system. For joint surgery such as artificial joint replacement and spine surgery, we devised treatments that can be expected to have maximum therapeutic effects with minimal invasiveness, prevent the occurrence of complications as much as possible, and enable early rehabilitation. We also provide appropriate surgery and treatment for injuries to the musculoskeletal system caused by traffic accidents, work-related accidents, sports, etc.
<About medical treatment features>
We have a system that can handle all kinds of Orthopedic Surgery diseases and injuries, such as hip joint surgery, knee joint surgery, rheumatism surgery including artificial joint replacement, spine surgery, upper limb surgery (microsurgery), and sports orthopedics.
In addition to hand surgery diseases, we also deal with shoulder joint diseases and elbow joint diseases. We also perform arthroscopic surgery for various joint diseases.
<Regarding Orthopedic Surgery training>
Since Kobe City hospital is in charge of tertiary emergencies, there are many cases of multiple injuries, spinal cord injuries, Orthopedic Surgery, and severe infections. I'm here. If you would like to have specialized training in Orthopedic Surgery at our hospital, please read "Regarding specialized training in Orthopedic Surgery". Also, please refer to the "Senior Resident Program / Recruitment Guidelines" from the "Recruitment Information" site.
In the "Kobe City Municipal Medical Center Orthopedic Surgery Specialized Training Program", our hospital will be the core facility, and the Kobe City Municipal Medical Center Nishi Municipal Hospital and Nishi Kobe Medical Center will be partner facilities. In addition to these three hospitals, the National Hospital Organization Himeji Medical Center, Hyogo Prefecture Amagasaki General Medical Center, Toyooka Public Hospital Association Toyooka Hospital, Social Medical Corporation Shinko Memorial Association Shinko Memorial Hospital, and Kyoto University are joint facilities. join the program.
Our department deals with many acute and chronic diseases including trauma. Each case is jointly handled by a Senior Resident in charge and a doctor in charge of each field, and it is possible to accumulate a wealth of experience.
We are planning to hold a special training program information session on June 3, 2022.
Introduction of 2017 Senior Resident Surgery Surgery Achievements
| spine | Upper limb/hand | Lower extremities | Trauma | rheumatism | sports | Child | tumor | others | |
| A. | 27 | 10 | 12 | 100 | 0 | 2 | 6 | 0 | 13 |
|---|---|---|---|---|---|---|---|---|---|
| B. | 30 | 15 | 60 | 90 | 0 | 0 | 15 | 10 | 0 |
| C. | 22 | 48 | 119 | 150 | 2 | 1 | 24 | 3 | 0 |
Impressions of Senior Resident about Orthopedic Surgery training
Senior Resident A
You can experience multiple injuries unique to tertiary emergency. I also feel that I can grow in a well-balanced manner after experiencing chronic diseases such as artificial joints and spine.
Senior Resident B
I feel that it is a privileged environment to experience many severe cases under the kind guidance of staff members who are well versed in their respective specialties. There are some difficult cases, but I am spending fulfilling days while being blessed with the same period and being encouraged. I actively participate in academic conferences and lectures, and have gained valuable experience. I would like to continue to devote myself to the training and put my feet on the ground.
Senior Resident C
At our hospital, we are able to experience a wide range of cases from the acute stage to the chronic stage under the backup of senior doctors. In particular, there are many complicated cases of trauma regardless of the body part, and I think that there are many cases that are very valuable as training because it is not only a simple procedure, but also training to make a solid preoperative plan. Also, regarding artificial joint surgery, you can be involved in surgery from an early stage, and you can gain experience in implant placement and cement procedures. Postoperative management also needs to be done in a responsible position as the attending physician, and I can feel that I am involved with the patient comprehensively. Therefore, I need to update my knowledge of not only Orthopedic Surgery but also other departments to some extent, which may be a little burdensome, but I think I am in an environment where I can grow as a doctor comprehensively. Senior doctors can equally handle duty and standby duty, so it is possible to devote holidays to your own time, and it is an environment that makes it easy to participate in seminars and academic conferences. I am full of gratitude to Director Yasuda and the other senior medical staff for providing me with training in an environment where I can learn both in classrooms and in practice at a high level.
Senior Resident D
I started my new post in October 2015. The specialized training at our clinic is still short, about 5 months, but I would like to write about two features of the training at our clinic.
The first is the ability to touch various wounds. Since our hospital focuses on emergency care, we will be in charge of various trauma cases. I thought I had experienced all kinds of injuries at the hospitals I worked at, but there were many cases that I had never experienced or that were difficult to treat.
The second is that you can learn about various specialized fields. Various cases have been introduced from Kobe City and surrounding areas. For example, during the 5 months of training, I had the experience of operating about 15 cases of THA. Among them, there are many difficult cases such as CDH and after Chiari surgery, and I am able to accumulate treatment experience that I can use in the future.
What makes this possible is that we have experts in each field who provide guidance and backup. I think it's wonderful to be able to do specialized training in such an environment. It's easy, but I wrote about the characteristics of the specialized training at our clinic.
Medical record
Departmental statistics
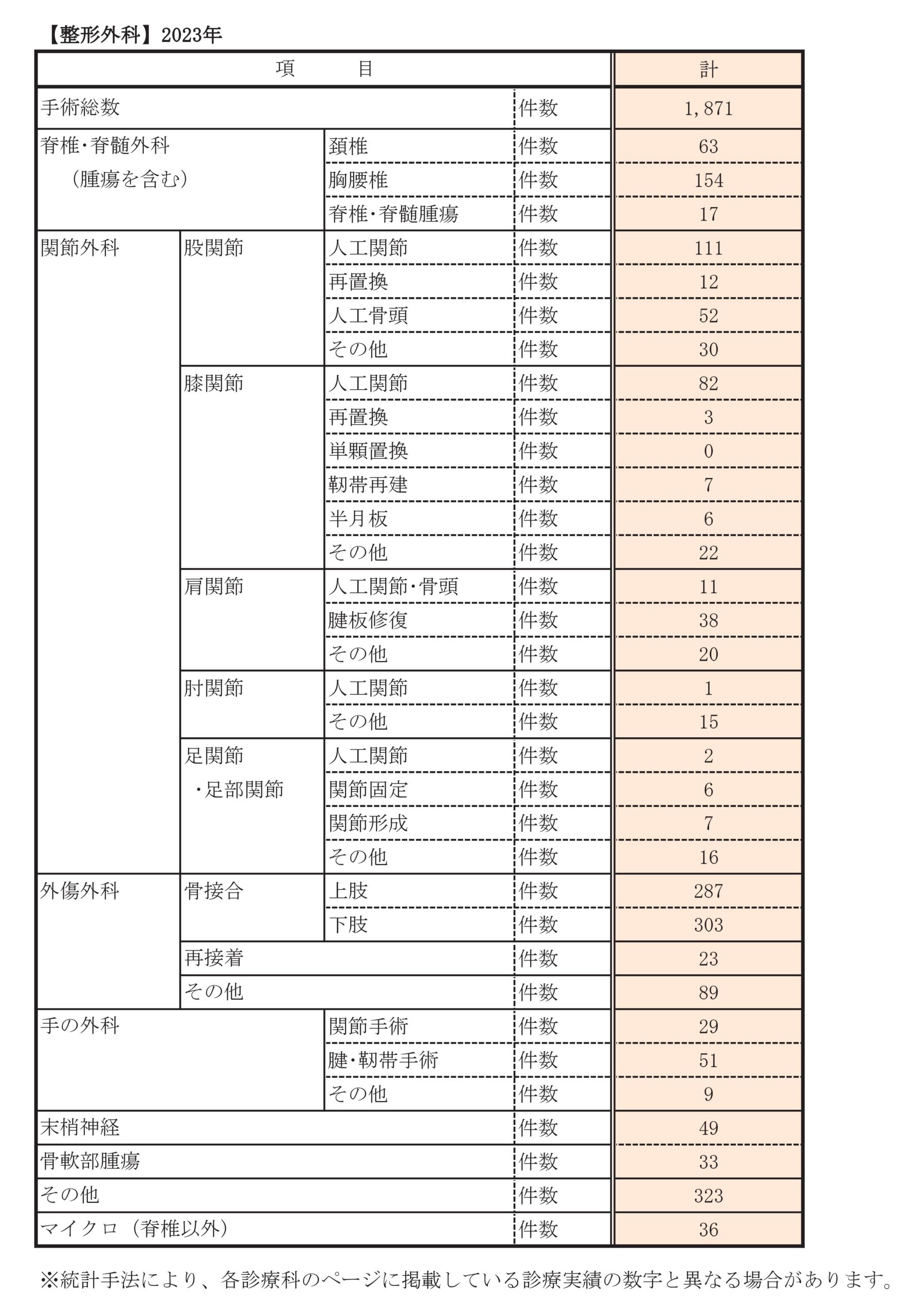
| 2014 | 2015 | 2016 | 2017 | 2018 | 2019 | 2020 | 2021 | 2022 | 2023 | |||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Spine/spinal cord surgery (including tumor) | cervical spine | 59 | 61 | 63 | 69 | 67 | 73 | 48 | 57 | 64 | 63 | |
| thoracolumbar spine | 86 | 127 | 102 | 127 | 144 | 164 | 110 | 149 | 150 | 154 | ||
| Spine/spinal cord tumor | 7 | 0 | 9 | 8 | 8 | 12 | 9 | 8 | 23 | 17 | ||
| joint surgery | hip joint | artificial joint | 85 | 70 | 102 | 94 | 104 | 129 | 90 | 86 | 93 | 111 |
| resubstitution | 15 | 15 | 14 | 16 | 14 | 20 | 12 | 11 | 19 | 12 | ||
| artificial femoral head | 38 | 48 | 42 | 41 | 49 | 41 | 28 | 33 | 49 | 52 | ||
| others | 22 | 18 | 27 | 38 | 25 | 27 | 15 | 29 | 24 | 30 | ||
| Knee joint | artificial joint | 79 | 81 | 83 | 78 | 75 | 75 | 54 | 40 | 51 | 82 | |
| resubstitution | 3 | 0 | 4 | 2 | 3 | 1 | 4 | 2 | 3 | 3 | ||
| Unicompartmental replacement | 0 | 3 | 0 | 0 | 5 | 16 | 11 | 4 | 3 | 0 | ||
| ligament reconstruction | 3 | 4 | 7 | 5 | 5 | 6 | 2 | 6 | 7 | 7 | ||
| meniscus | 14 | 8 | 22 | 33 | 16 | 17 | 7 | 6 | 8 | 6 | ||
| others | 18 | 24 | 44 | 22 | 31 | 27 | 33 | 30 | 20 | 22 | ||
| shoulder joint | Artificial joint/head | 2 | 4 | 9 | 8 | 9 | 5 | 12 | 7 | 9 | 11 | |
| rotator cuff repair | 1 | 7 | 10 | 14 | 20 | 18 | 14 | 23 | 24 | 38 | ||
| others | 7 | 6 | 7 | 6 | 6 | 14 | 14 | 20 | 14 | 20 | ||
| elbow joint | artificial joint | 1 | 2 | 6 | 1 | 5 | 0 | 2 | 2 | 1 | 1 | |
| others | 2 | 4 | 4 | 4 | 6 | 11 | 7 | 11 | 7 | 15 | ||
| Ankle joint/Foot joint | artificial joint | 0 | 0 | 0 | 0 | 1 | 0 | 2 | 0 | 0 | 2 | |
| arthrodesis | 1 | 2 | 2 | 6 | 4 | 5 | 1 | 1 | 2 | 6 | ||
| arthroplasty | 3 | 2 | 2 | 5 | 1 | 3 | 4 | 4 | 5 | 7 | ||
| others | 4 | 6 | 4 | 5 | 10 | 8 | 17 | 12 | 19 | 16 | ||
| trauma surgery | osteosynthesis | upper limbs | 210 | 211 | 237 | 253 | 279 | 289 | 183 | 244 | 283 | 287 |
| Lower extremities | 196 | 211 | 250 | 239 | 255 | 272 | 176 | 255 | 324 | 303 | ||
| re-adhesion | 33 | 25 | 26 | 35 | 23 | 30 | 20 | 27 | 28 | 23 | ||
| others | 105 | 110 | 88 | 292 | 249 | 121 | 81 | 70 | 79 | 89 | ||
| hand surgery | joint surgery | 16 | 16 | 18 | 24 | 17 | 20 | 17 | 27 | 38 | 29 | |
| Tendon/ligament surgery | 58 | 48 | 56 | 55 | 60 | 71 | 47 | 53 | 57 | 51 | ||
| others | 8 | 21 | 14 | 12 | 5 | 6 | 7 | 12 | 4 | 9 | ||
| peripheral nerve | 37 | 53 | 45 | 49 | 46 | 66 | 56 | 37 | 46 | 49 | ||
| Bone and soft tissue tumor | 31 | 49 | 46 | 35 | 31 | 37 | 32 | 30 | 23 | 33 | ||
| others | 187 | 198 | 223 | 56 | 29 | 235 | 158 | 162 | 237 | 323 | ||
| Micro (non-spine) | 48 | 57 | 57 | 67 | 48 | 49 | 38 | 40 | 59 | 36 | ||
| Total number of surgeries | 1331 | 1434 | 1566 | 1632 | 1602 | 1819 | 1273 | 1458 | 1714 | 1871 | ||
Main diseases/treatments
hip surgery
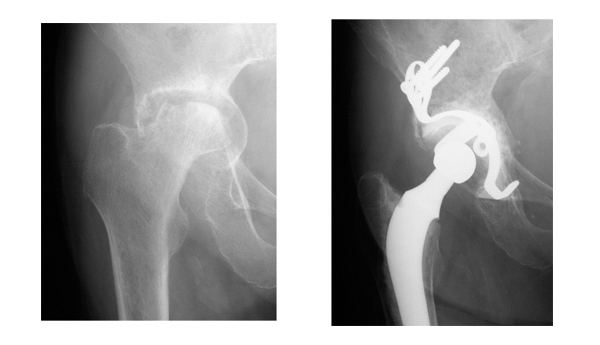
We perform surgeries for hip osteoarthritis, femoral head necrosis, acetabulum dysplasia, hip labrum injury, etc.
Hip replacement surgery for hip osteoarthritis and femoral head necrosis can reduce pain in the hip joint and allow more freedom of activity and movement. In addition, if there is a difference in the length of the left and right legs, the length of the left and right can be almost the same, so the burden on the knees and lower back can be reduced, and the gait (walking) can be improved considerably. After surgery, some people enjoy swimming, walking, golf, cycling, light mountain climbing, and tennis. However, complications include postoperative infection and dislocation. The incidence rate is about 1% for both cases, but we pay close attention to its prevention and countermeasures.
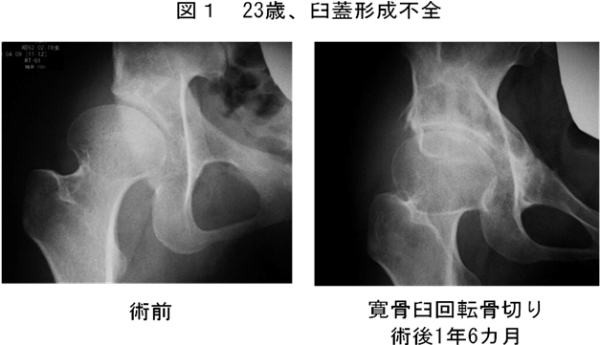
Acetabuloplasty and acetabular rotation osteotomy for acetabulum dysplasia, femoral head rotation osteotomy for femoral head necrosis, and hip arthroscopic surgery for hip labrum injury. both have achieved good results.
Osteoarthritis of the hip
Surgery using your own bone
Since articular cartilage has poor self-repair ability, the surgical method differs depending on whether the articular cartilage remains undegenerated or degenerated and worn out. If articular cartilage remains, surgery to preserve the bones and joints, such as acetabuloplasty and acetabular rotation osteotomy, is the mainstay. It was found that young people up to the age of 25 had better long-term results in acetabuloplasty (shelfoplasty) than older people. Acetabuloplasty improves the fit of the hip joint in younger people. However, it is not performed when cartilage wear has progressed to some extent. We believe that acetabuloplasty is indicated for people under the age of 25 who do not have articular cartilage degeneration. On the other hand, we believe that rotation acetabular osteotomy is indicated for people up to the age of 50, when joint compatibility improves when the hip joint is opened outward, even if cartilage degeneration has begun (Fig. 1). ). In both cases, the hospitalization period is 1 to 1.5 months, and it is necessary to wait about 3 months after the operation until bone union is obtained before returning to light work.
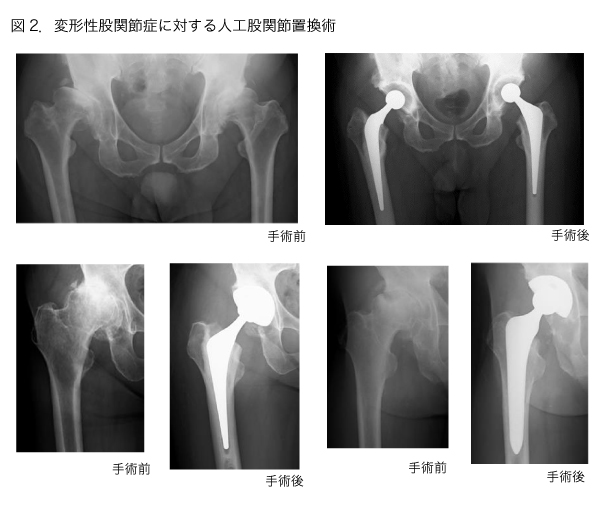
total hip arthroplasty
If the cartilage degeneration progresses and wears out, and the hip joint has poor movement or the length of the leg is shortened, surgery to replace it with an artificial hip joint is indicated. The hospital stay is about 2 weeks. Continuing rehabilitation after surgery. Depending on each person's living environment and preoperative conditions, you will be able to lead a normal life in about 1 to 2 months. There is no strict age limit, as people in their 20s can undergo surgery if there is no other way to improve function other than total hip replacement surgery, and people over 80 can undergo surgery if there are no serious complications. We have excellent staff in all clinical departments, so we have established a system where even patients with various complications can undergo surgery with peace of mind. Also, by collecting the blood that bleeds after surgery and returning it to the patient, there is no need to store your own blood before surgery. The operation is a combination of general anesthesia and continuous epidural anesthesia, so you can spend almost no pain for 2 days after the operation. Another feature of our facility is that there are many excellent physical therapists in charge of rehabilitation. Standing and walking training begins the day after surgery. Physical therapists on duty are basically in charge of rehabilitation on Saturdays and Sundays. After about two weeks, some patients are able to walk with a cane and can go home, while others are transferred to other hospitals and continue their rehabilitation. If you live alone or it seems that it will take time to adjust to your daily life, we will make a reservation to transfer to a partner hospital before surgery.
The artificial joint to be used is determined according to the condition of each patient's hip joint.
We cooperate with the artificial joint registration system of the Japanese Society for Artificial Joints.After the artificial joint surgery, you will have regular follow-up visits to monitor your progress.
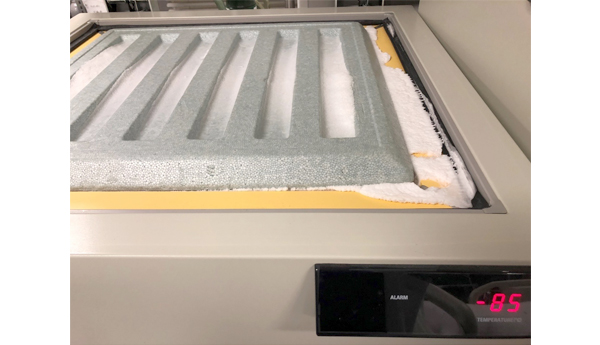
Revision hip arthroplasty (replacement surgery)
Approximately 20% of cases require replacement surgery 20 years after surgery due to loosening of the joint between the artificial joint and the bone. The two-week hospitalization is almost the same as the first artificial joint surgery, so it can be said that the burden on the patient has been greatly reduced compared to before. However, revision surgery is by no means a simple operation. The patient is older than the initial surgery, and there are concerns about deterioration of cardiopulmonary function and various systemic complications, as well as bone fragility, bone loss, muscle atrophy, scar formation from the initial surgery, and changes in anatomical structure. Various difficulties and problems must be resolved. In particular, it is a big problem that fixation tends to be insufficient due to bone defects. We have a bone bank at -80°C in our hospital in preparation for allogeneic bone grafting for bone defects (Fig. 3). Although some hospitals called artificial joint centers do not have a bone bank, in most of the revision surgeries we perform, allogeneic bone grafting is performed from a bone bank (Fig. 4). Even if the patient is elderly, since our hospital is a general hospital, a specialist intensive care doctor is always present in the intensive care unit, and high-risk patients are treated in cooperation with other departments such as cardiology and respiratory medicine. You can also accept Reoperation allows you to return to your normal life, so you will never be in a wheelchair if the artificial joint loosens.
knee joint surgery
Regarding knee joints, we treat knee joint dysfunction caused by osteoarthritis and rheumatoid arthritis, and meniscal and anterior cruciate ligament injuries caused by sports injuries.
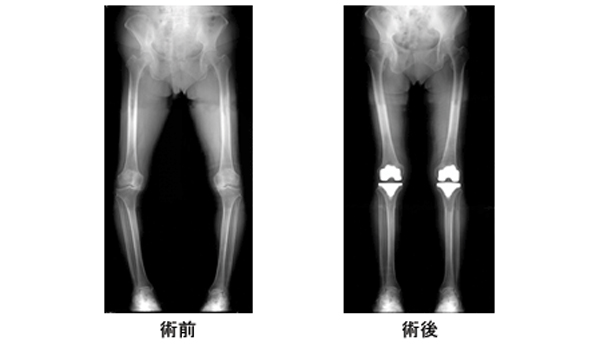
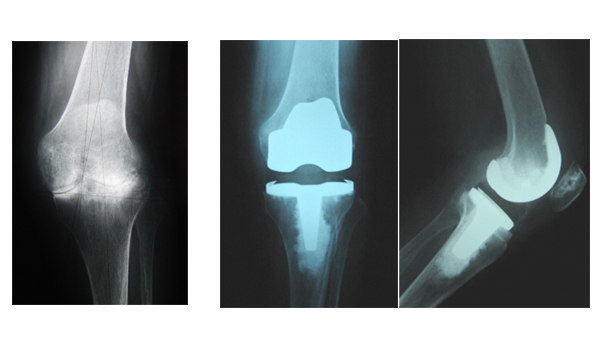
As Japan transitions to an aging society, the number of patients suffering from knee osteoarthritis is increasing year by year. For knee osteoarthritis, rheumatoid arthritis, and intra-articular osteonecrosis of the knee, total knee arthroplasty (TKA) may be recommended if the pain worsens despite drug therapy such as joint injections, making daily activities difficult. , unicompartmental arthroplasty (UKA), and high tibial osteotomy (HTO).
knee osteoarthritis
The smooth and elastic articular cartilage that covers the surfaces of the femur, tibia, and patella of the knee joint degenerates due to aging, obesity, trauma, etc., and the cartilage gradually wears away. will result in osteoarthritis of the knee. When you bend or straighten your knee, when you walk, or when you go up or down stairs, you may experience pain, and it becomes difficult to bend and straighten your knee. The function of the knee joint gradually deteriorates, making it difficult to perform daily activities, and the joint deforms. Also, when the symptoms are severe, fluid may accumulate in the joint. Rheumatoid arthritis also destroys the cartilage and bones of the knee joints due to inflammation, causing pain, deformation, and functional disorders, which interferes with activities of daily living.
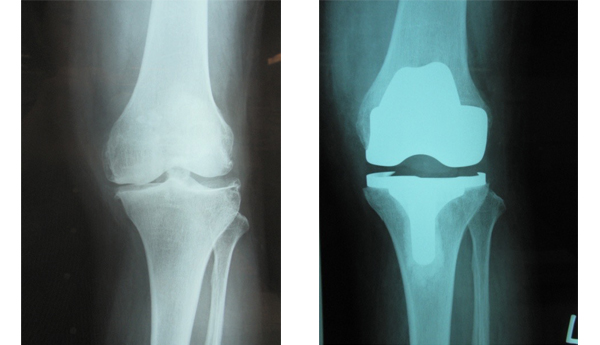
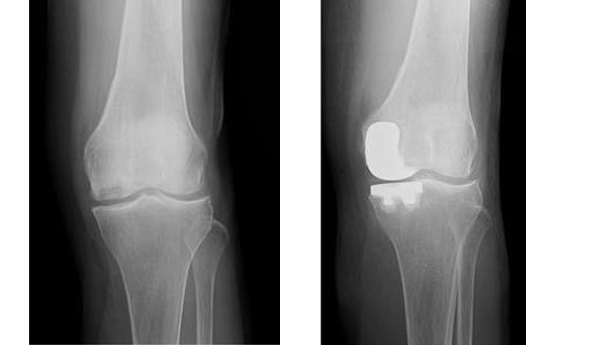
total knee arthroplasty
For knee osteoarthritis, do not perform conservative surgery such as exercise therapy such as quadriceps femoral muscle training, topical agents such as poultices and ointments, oral anti-inflammatory analgesics, and intra-articular injection of hyaluronic acid. Treat first. If the knee joint dysfunction still does not improve, a total knee arthroplasty (TKA) is performed. TKA is also performed when functional impairment due to rheumatoid arthritis is severe. TKA is a surgical procedure in which a damaged joint is removed and replaced with an artificial joint. It is a very good surgery with a great pain-relieving effect because it removes everything that causes pain in the joints. In addition, TKA corrects deformities (bow legs and bow legs), resulting in straight knees (Figs. 1 and 2). However, even if you undergo TKA, it is difficult to bend your knees enough to sit straight, but there is no problem in your daily life other than sitting straight. Light exercise such as walking, swimming, and cycling on flat ground is possible. You cannot participate in strenuous sports such as running or soccer.
Artificial knee joints are made of materials such as titanium alloys and high molecular weight polyethylene. After surgery, there is no problem with MRI examination. Once the surgery is performed, in most cases, the artificial knee joint will not need to be replaced for the rest of its life.
The hospital stay is about 2 weeks. Continuing rehabilitation after surgery. After 2 to 3 months, you will be able to lead a normal daily life. If there are no serious complications, the operation can be performed even if the patient is over 80 years old, and there is no strict age limit. We have excellent staff in all clinical departments, so we have a system in place that allows even patients with various complications to undergo surgery. Also, because hemostats are used during surgery, the chance of transfusion is less than 3%. The operation is a combination of general anesthesia and block injection, so you can spend two days after the operation without feeling much pain. The operation takes about 2 to 3 hours, and walking training begins the day after the operation, and on the 3rd day after the operation, the patient is able to go to the toilet by himself in a wheelchair. You can walk with a cane in 2 weeks. Two weeks after surgery, the patient was transferred to a rehabilitation hospital for rehabilitation purposes. After about one month of rehabilitation treatment (gait training, leg strength training, knee range of motion training) at a rehabilitation hospital, the patient will be discharged.
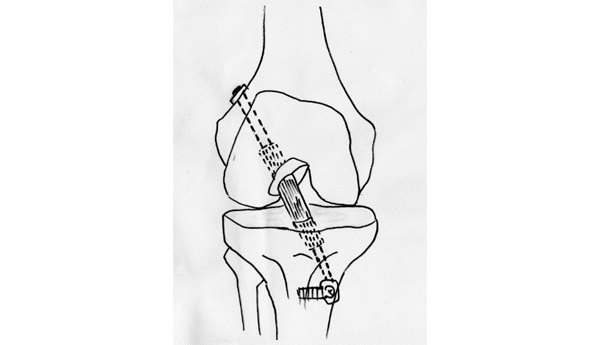
High tibial osteotomy (HTO)
High tibial osteotomy is recommended for relatively young people with bow leg deformity, intra-articular osteonecrosis of the knee, active people, and those who do sports or heavy work. Unlike TKA, heavy work and sports are possible after surgery. It is a surgery to reduce the burden on the inside of the knee joint due to the bow leg by correcting the bow leg by cutting the tibia. A wedge-shaped osteotomy is performed on the inner side of the proximal tibia, and artificial bone is implanted and fixed with a titanium alloy plate and screws. A tibial osteotomy corrects the bow leg to a normal bow leg. Wheelchair movement is possible from the day after surgery. About 2 weeks after the operation, full-weight walking will start, and about 3 weeks after the operation, you will be discharged from the hospital with walking sticks. Light exercise such as hiking and golf can be resumed after 3 to 4 months, and heavy work and sports such as running can be resumed after 9 to 12 months. The fixation bracket is removed approximately one year after surgery (Fig. 3).
Unicompartmental knee arthroplasty (UKA)
meniscus injury
The meniscus is a fibrous tissue between the femur and tibia. The medial meniscus is C-shaped and the lateral meniscus is semicircular. Involved in knee joint load distribution, support stability function, and joint movement. Meniscal injuries are common during the late teens and early twenties when people are physically active, including playing sports. The meniscus is often damaged during imbalanced movements such as soccer and basketball. After the age of 40, age-related degeneration of the meniscus can lead to tearing, even without trauma.
The meniscus does not show up on x-rays. Therefore, MRI examination is necessary to make a diagnosis of meniscal injury. MRI examinations are harmless and painless. An MRI scan can show the condition of the meniscus and ligaments.
For meniscal injuries, we first monitor the progress with analgesics, topical agents, intra-articular injections, etc. Arthroscopic surgery is done if the pain does not improve, or if MRI reveals a significant tear. Since the camera is inserted into the joint during the surgery, the scar is small. Depending on the type of tear, a meniscal tear is excised if it cannot be sutured, and sutured if sutured.
The surgery is performed under spinal anesthesia (lower body anesthesia). If resection is performed, hospitalization is about 2 to 4 days, walking is possible from the next day, and the return to heavy work is about 2 to 3 months. If suturing is performed, the patient will need to be hospitalized for about 1 to 2 weeks and be immobilized in a cast for about 3 to 4 weeks, and it will take about 4 to 6 months before returning to heavy work.
anterior cruciate ligament injury
Anterior cruciate ligament injuries are among the most common knee sports injuries. It occurs during sports such as jump landings, takeoffs, sudden stops, and sudden changes in direction. It can also occur in contact sports, such as rugby and judo, when the knee is twisted in contact with an opponent.
Diagnosis of anterior cruciate ligament injury is made by interview, examination findings, and MRI examination.
spine surgery
There are a wide variety of spinal diseases, and along with recent advances in spinal surgery, there are various options for actual treatment methods. At our clinic, we focus on making an accurate diagnosis and selecting the appropriate treatment for it. The principle of treatment is conservative treatment, and if there is no movement disorder or significant pain in the limbs, outpatient drug therapy, nerve block treatment, rehabilitation treatment, etc. are performed (outpatient rehabilitation is difficult at our hospital, so appropriate at the facility). However, if the symptoms cannot be resolved without surgery, surgical treatment should be considered.
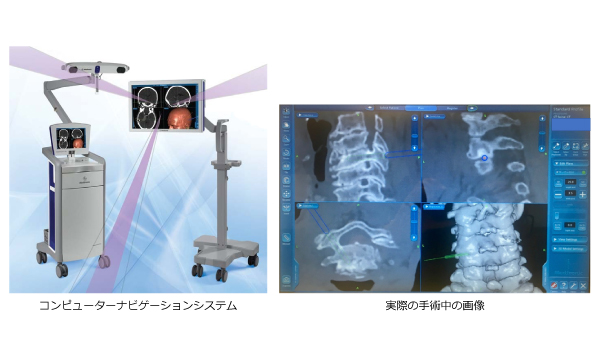
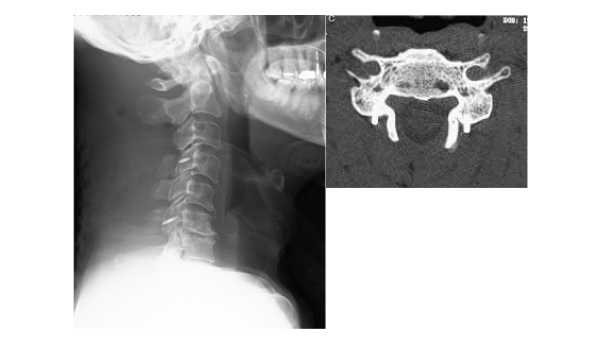
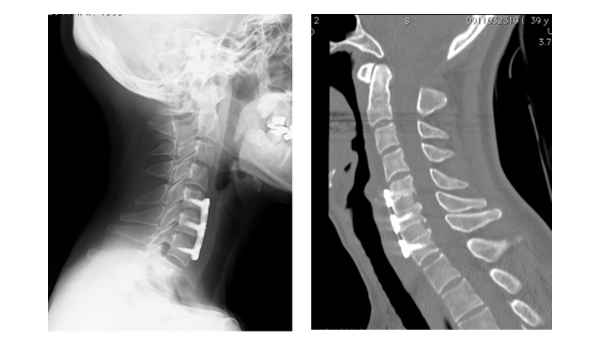
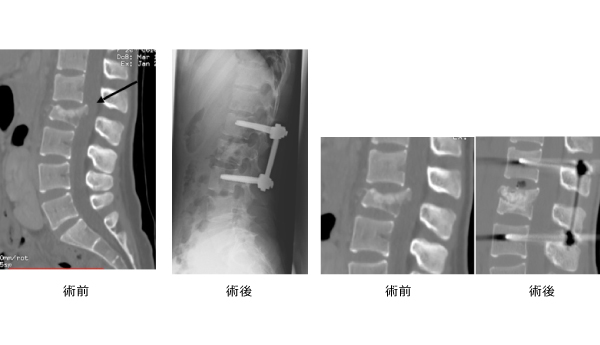
Spine surgery performed at our hospital includes surgery for degenerative diseases such as aging and rheumatism, and surgery for trauma such as falls and traffic accidents. For spinal metastasis of cancer, we perform surgical treatment for the purpose of relieving symptoms such as early social reintegration and paralysis and pain. In order to perform optimal and safe treatment, we have introduced a computer navigation system at our hospital, which enables accurate placement of implants even in cervical spine instrumentation surgery and cases of advanced spinal deformity (Fig. 1). ). In addition, the number of patients with various complications is increasing with the aging society. It is possible to have surgery with peace of mind.
At our hospital, we treat most spinal diseases other than intramedullary tumors, but the typical diseases are as follows.
cervical spine
Cervical spondylotic myelopathy, cervical disc herniation, cervical radiculopathy, posterior longitudinal ligament ossification, atlantoaxial subluxation (rheumatoid arthritis)
thoracolumbar spine
Lumbar spinal canal stenosis, lumbar spondylolisthesis, lumbar spondylolisthesis, degenerative scoliosis, disc herniation, posterior longitudinal ligament ossification, ligamentum flavum ossification, adult spinal deformity
others
Spinal cord tumor (excluding intramedullary tumor), spinal tumor, metastatic spinal tumor, spinal compression fracture, fracture/dislocation/spinal cord injury due to trauma
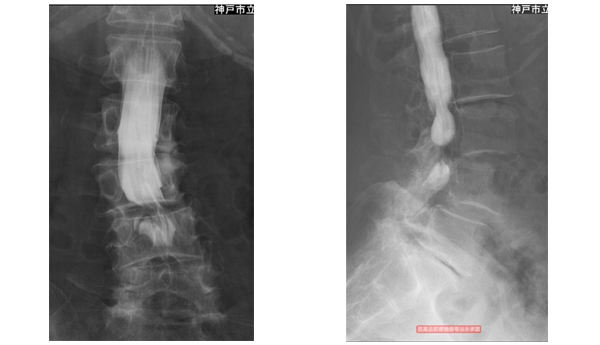
Lumbar spinal stenosis
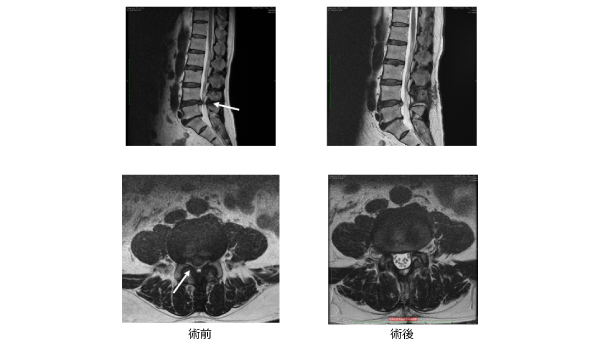
Diagnosis includes CT, MRI, myelography, and nerve root blocks that paralyze certain nerves. For foraminal stenosis and extraforaminal stenosis, which are difficult to diagnose, we perform accurate diagnosis using 3D MRI, nerve root block, and contrast-enhanced CT.
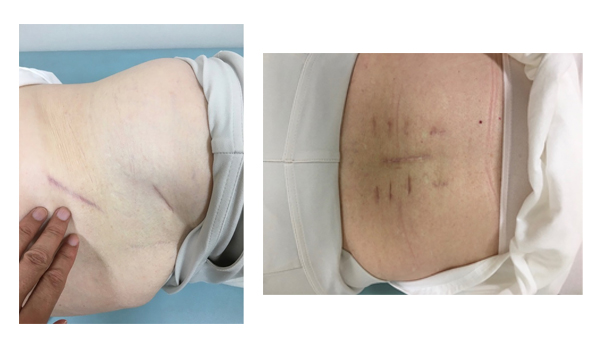
Conservative treatment includes oral medication and nerve block therapy. Surgery may be necessary if conservative treatment fails to improve symptoms. In the case of normal spinal canal stenosis only, we use the minimally invasive spinal process splitting method, which is performed under a microscope with an approach that minimizes damage to the muscles of the lower back. The skin incision is small, about 4 cm, and the patient is usually able to walk the next day (Fig. 2). If there is misalignment of the lower back bones (lumbar spondylolisthesis), if there is scoliosis, or if foramen stenosis is suspected, spinal fusion may be added. A metal implant is used for fixation, but depending on the case, a percutaneous pedicle screw is used to make it less invasive (Fig. 3).
OLIF: A minimally invasive lumbar fusion surgery that is becoming popular in Japan, in which a cage is inserted between the vertebral bodies through a skin incision of approximately 5 cm from the flank. It is effective in correcting degenerative scoliosis and spinal misalignment (Fig. 3).
Lumbar disc herniation
Symptoms improve in most cases with oral treatment and nerve block therapy. If there is muscle weakness or significant pain, or if early rehabilitation is required, surgical treatment is selected. Microscopic herniectomy is performed using a skin incision of approximately 3-4 cm.
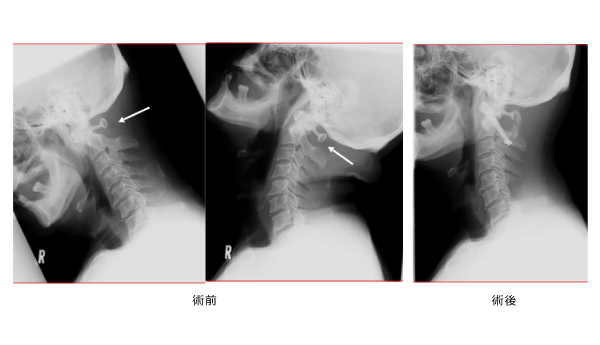
cervical myelopathy
It is a condition caused by the compression of the spinal cord by the cervical vertebrae. Symptoms include difficulty in fine hand movements and difficulty in walking.
At our hospital, the surgical method is selected according to the symptoms and condition of the patient. More than half of the patients undergo laminoplasty to remove pressure on the nerve from the back of the neck. It adopts a double-opening type that opens the vertebral arch to the left and right. You will be able to walk while wearing a collar from the early postoperative period. In addition, we perform anterior cervical decompression fixation when there is a pressure element of the spinal cord in front (Fig. 4).
The area around the cervical spine contains not only the spinal cord but also large blood vessels such as the vertebral arteries, so extreme caution is required. At our hospital, we perform blood vessel evaluation with contrast-enhanced CT before surgery as necessary, and perform safe and accurate surgery using a computer navigation system during surgery.
After surgery on the cervical spine, the whole body is managed in the intensive care unit, and after confirming that there are no problems, the patient is sent back to the ward.
Atlantoaxial subluxation/instability
surgery for trauma
Surgery for metastatic spinal tumors
When a malignant tumor such as cancer metastasizes to the spine, it compresses the spinal cord and causes paralysis. If the life prognosis is long and the progression of paralysis is minor, the paralysis can often be improved by releasing the spinal cord pressure and immobilizing it. In addition, when the metastatic focus is solitary, tumor resection may be performed for the purpose of radical intellectual treatment.
Minimally Invasive spine Stabilization (MISt)
In spinal surgery, we aim to perform minimally invasive surgery as much as possible to achieve early rehabilitation, less bleeding, and less postoperative pain. At our hospital, we apply MISt surgery not only to normal spinal surgery, but also to surgery for metastatic spinal tumors and spinal trauma. Compared to conventional incision surgery, it has been proven that the amount of bleeding during and after surgery is less. Since there is little burden on the body, early rehabilitation after surgery is possible.
upper extremity surgery
In today's world of computers and mobile phones, hands are indispensable for daily life, and if the functions of the hands are impaired, human life will be greatly restricted. In addition, since the hand is useful only when it is linked to the movement of the shoulder and elbow joints, it is important to treat disorders and diseases of the entire upper extremity in a well-balanced manner in hand surgery.
Since the hand is an anatomical structure with a dense collection of various tissues such as bones, cartilage, ligaments, tendons, nerves, blood vessels, and skin, even a seemingly simple injury such as a cut with a kitchen knife can damage nearby tissues. In many cases, the treatment requires specialized knowledge and techniques such as microsurgery. In addition, endoscopic techniques are becoming more important in the treatment of shoulders and elbows in order to perform treatments based on less invasive and more accurate diagnoses. Our hospital's upper extremity surgery department aims to provide integrated treatment with three major pillars: the general hand surgery department, the micro-reconstruction department, and the shoulder and elbow sports department. We introduce typical upper extremity surgical diseases treated in our department.
carpal tunnel syndrome
When the median nerve is compressed in the space called the carpal tunnel on the palm side of the wrist, you will become aware of numbness in your fingertips. In a typical example, numbness often wakes up at night, and as it progresses, the muscle at the base of the thumb weakens, making fine movements difficult.
As a treatment, conservative treatment such as a night brace is performed first, but if there is no effect or if it progresses, surgery to remove the pressure in the carpal tunnel (carpal tunnel release) is performed.
There are two types of surgery, direct open surgery and arthroscopic open surgery using a 4 mm diameter arthroscope, and the surgical method is determined according to the patient's wishes. Arthroscopic treatment is often performed because the scar is relatively small and there is little postoperative pain (Fig. 1). Both methods require local anesthesia and the operation takes about 10 to 20 minutes, so it is possible to undergo the procedure as a day surgery.
Distal radius fracture
The radius is the bone on the thumb side of the two bones in the forearm (between the elbow joint and the wrist joint), and fractures near the wrist joint occur frequently when a person falls and falls on the hand, especially in elderly women. It is a common fracture in people with osteoporosis. Leaving a large dislocation at the fracture site not only causes pain in the wrist joint, but also causes functional disorders in parts other than the wrist joint, such as restricted supination and supination of the forearm. will be left. As a treatment, if the dislocation is small, immobilization with a cast is performed, but if there is a large dislocation or if the fracture is unstable even after manual reduction, surgery is required. In recent years, due to the growing awareness of healthy life expectancy, many elderly patients are choosing surgical treatment so as not to impair the original movement of the wrist joint as much as possible. Surgery mainly involves internal fixation using a palmar locking plate. The locking plate, which has been developed in recent years, has a structure in which the plate and screw are integrated, providing strong fixing force and enabling early return to society (Fig. 2). The operation is conducted under conduction anesthesia (injection into the base of the arm, anesthesia for only the upper extremities undergoing surgery), and the operation takes about an hour. It is possible to receive it in hospital for 1 night and 2 days, and the skin incision is only about 6 cm. In order to allow the patient to return to normal life as soon as possible, we try to plan the surgery within a few days as long as the operating room is available.
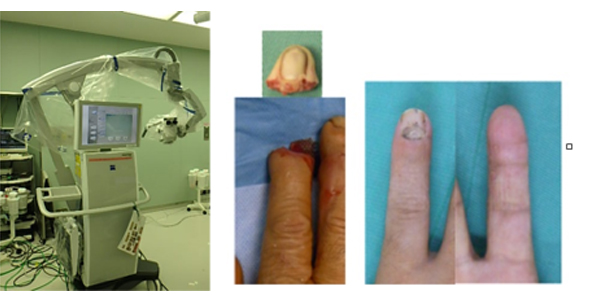
Finger Amputation/Microsurgery
Since the world's first successful reattachment of a mother's finger for complete amputation in Japan in 1965, Japanese microsurgery and hand surgery techniques have been highly regarded overseas. Surgery to restore blood flow to an amputated finger requires urgency and requires specialized knowledge and skills due to the combined damage to bone, tendons, nerves, blood vessels, and skin. The first re-attachment surgery in our hospital was performed in 1972, which is already nearly half a century old. Amputation finger treatment requires not only medical equipment such as operating microscopes, but also the cooperation of the emergency department, operating room, and Anesthesiology. Although there was a time when we could not accept patients due to changes in the medical treatment system, we currently perform about 30 amputation finger reattachments every year based on our original philosophy of practicing 24-hour emergency medicine, and accept patients not only from Hyogo Prefecture but also from other prefectures as much as possible (Fig. 3). We perform about 90 microsurgeries a year, including not only amputated fingers but also free tissue grafts and peripheral neuropathies using microscopes.
Shoulder joint endoscopic treatment
In recent years, endoscopic treatment has become indispensable for improving diagnostic accuracy and treatment outcomes in shoulder surgery. The main diseases for which endoscopic treatment is performed include shoulder rotator cuff tear and shoulder joint dislocation (labrum injury).
A rotator cuff tear is a disease that causes symptoms such as pain in the shoulder joint and inability to raise the arm. A torn rotator cuff can make your shoulders weak, make it difficult to put on and take off your clothes, and keep you from sleeping because of the pain. Basically, we aim to cure without surgery such as rehabilitation and injections, but surgery may be performed depending on the severity of symptoms and the duration of illness. Although postoperative immobilization rehabilitation is required, we aim to improve pain by smoothing the movement of the shoulder joint, which requires three-dimensional movement. Endoscopic labrum suture has become the standard treatment for recurrent shoulder joint dislocations. Anterior braking with bone grafting may be performed, but endoscopic treatment is performed with as little burden as possible.
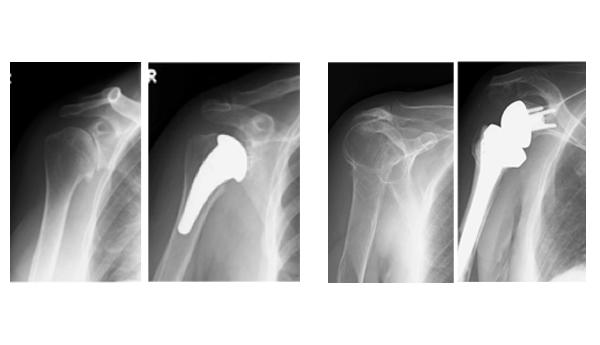
shoulder prosthesis treatment
Until now, the theme of artificial shoulder joints was how to reproduce the three-dimensional three-dimensional movement unique to the shoulder while maintaining the anatomical structure. is happening. Indications are limited to the elderly, where reconstruction is more difficult, but it has become reasonably successful in osteoarthritis of the shoulder with large rotator cuff tears and comminuted humeral fractures with difficult osteosynthesis. rice field. At our hospital, we give priority to endoscopic treatment and try to preserve the joint as much as possible.
rheumatoid arthritis surgery
When rheumatoid arthritis destroys joints, it causes pain, swelling, and dysfunction. Surgery may be needed to restore joint function.
hip joint
Knee joint
ankle joint

elbow joint

others
We also perform finger, wrist, shoulder and foot surgery.
trauma Orthopedic Surgery
Our hospital was the first emergency medical center to be certified in Japan, and for four consecutive years since 2014, we have been ranked No. Currently, we accept more than 10,000 emergency cases per year. Half of Orthopedic Surgery surgeries (approximately 800 in 2017) are temporary or emergency surgeries, and are characterized by an extremely large number of trauma cases associated with life-saving emergencies. There are many cases of serious injuries, and the range of injuries is wide-ranging, including spine, joints, hand surgery cases requiring microsurgery, and complex tissue injuries requiring soft tissue reconstruction. Depending on the case, specialists in each field work together to provide medical care with the goal of restoring function and returning to social life. Some of the characteristic trauma cases in our department are shown below.
There are many cases of serious injuries, and the range of injuries is wide-ranging, including spine, joints, hand surgery cases requiring microsurgery, and complex tissue injuries requiring soft tissue reconstruction. Depending on the case, specialists in each field work together to provide medical care with the goal of restoring function and returning to social life. Some of the characteristic trauma cases in our department are shown below.
pediatric fracture
Pediatric fractures are mainly seen around the elbow joint, often in the forearm and also in the lower extremities. In principle, in cases with dislocation, internal fixation surgery is performed on the same day. In 2017, we performed 29 surgeries for fractures in children under 15 years of age (Figures 1-3).
open fracture
It occurs most often in the tibia, but can also occur in the forearm and femur. Since the risk of infection is high and early cleaning and debridement are required, emergency surgery is performed. There are many cases with extensive skin and soft tissue defects, and we are consistently working on reconstruction. In 2017, we performed 13 surgeries for open tibia fractures alone (Figures 4 and 5).
spinal trauma
It ranges from dislocated fractures associated with high-energy trauma to non-bone traumatic spinal cord injuries. Some cases require emergency measures such as reduction, fixation and decompression. (See spine surgery section)
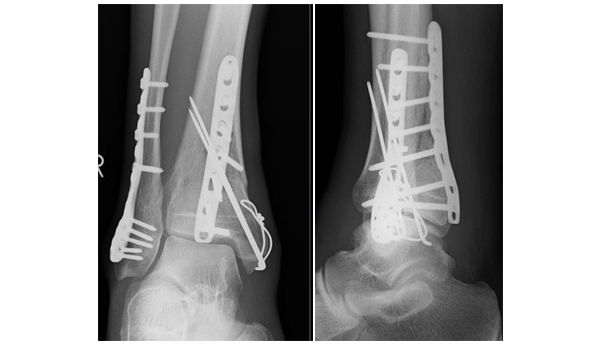
intra-articular fracture
There are many fracture cases with destruction of not only the normal diaphyseal shaft but also the articular surface due to high-energy trauma. Perform anatomical reduction whenever possible. (Figures 6-8)
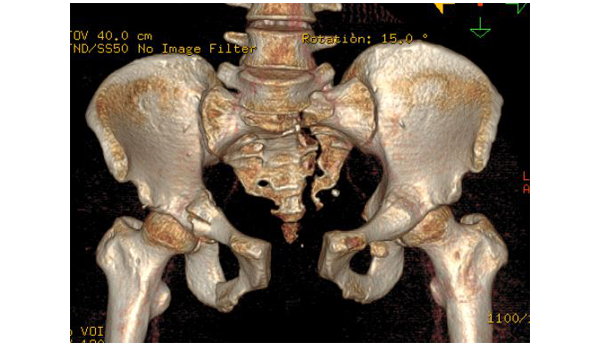
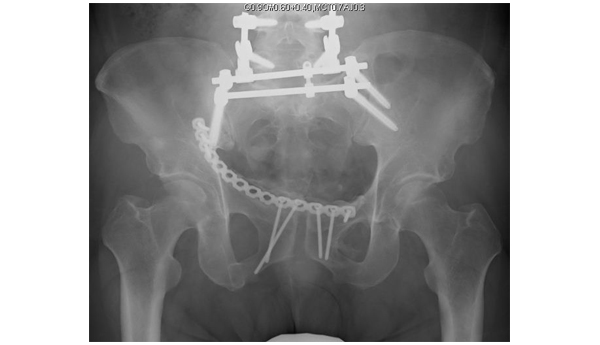
pelvic fracture
There are about 50 cases of emergency transportation per year. The initial response is to perform arterial embolization very early, showing a good survival rate. With an emphasis on functional prognosis, we perform surgical treatment for approximately 30 cases of dislocation and instability per year. (Figures 9 and 10)
surgery video
clinical research
Specified Clinical Research/FY2020 Katakami Clinical Research Grant
| Research subject | A study on the effect of 3-hydroxy-3-methylbutyrate on functional recovery after total hip arthroplasty and total knee arthroplasty in the elderly with osteoarthritis |
|---|---|
| Research representative | Yoshi Yasuda |
2019 Katakami Clinical Research Grant
| Research subject | Elucidation of the involvement of Stat3 in joint destruction in rapidly destroying hip arthritis - toward clinical application of anti-Stat3 drugs |
|---|---|
| Research representative | Yoshi Yasuda |
Published paper
- Yasuda T, Hara S, Yamashita S, Mitsuzawa S, Tsukamoto Y, Takeuchi H, Ota S, Onishi E. Activation of STAT3 (signal transducer and activator of transcription 3) in synovial tissues from the hip joint in the early stage of rapidly destructive coxopathy. Biomedical Research (Tokyo). 2022; 43(5): 173-180.
2019 The Hyogo Prefecture Medical Association Medical Research Grant
| Research subject | Research on the effects of hip and femoral muscles on functional recovery after total knee arthroplasty and total hip arthroplasty |
|---|---|
| Research representative | Yoshi Yasuda |
Published paper
- Yasuda T, Honda S, Matsunaga K, Hashimura T, Tsukamoto Y, Ota S, Fujita S, Onishi E. Association of preoperative muscle composition of the lower extremity with gait function after total knee arthroplasty. J Orthop Sci. 2023; 28(1) ): 188-194.
- Yasuda T, Ota S, Yamashita S, Tsukamoto Y, Onishi E. Association of preoperative variables of ipsilateral hip abductor muscles with gait function after total hip arthroplasty: a retrospective study. Arthroplasty 2022; 4: 23.
- Yasuda T, Ota S, Mitsuzawa S, Yamashita S, Tsukamoto Y, Takeuchi H, Onishi E. Preoperative lower-limb muscle predictors for gait speed improvement after total hip arthroplasty for patients with osteoarthritis. J. Pers. Med. 2023; 13: 1279.
2018 Hip Joint Research Grant
| Research subject | Establishment of early diagnostic method for rapidly destructive hip arthritis |
|---|---|
| Research representative | Yoshi Yasuda |
Published paper
- Yasuda T, Matsunaga K, Hashimura T, Tsukamoto Y, Sueyoshi T, Ota S, Fujita S, Onishi E. Bone turnover markers in the early stage of rapidly progressive osteoarthritis of the hip. European Journal of Rheumatology 2021; 8(2): 57-61.
- Yasuda T, Matsunaga K, Hashimura T, Tsukamoto Y, Sueyoshi T, Ota S, Fujita S, Onishi E. Characterization of rapidly progressive osteoarthritis of the hip in its early stage. European Journal of Rheumatology 2020 Jul;7(3):130 -134. DOI: 10.5152/eurjrheum.2020.19159.
- Yasuda T, Matsunaga K, Hashimura T, Tsukamoto Y, Sueyoshi T, Ota S, Fujita S, Onishi E. Characterization of Femoral Head Destruction in the Early Stage of Rapidly Progressive Osteoarthritis of the Hip. Austin Journal of Orthopedics & Rheumatology 2019; 6 (2): 1081.
- Onishi E, Ota S, Fujita S, Tsukamoto Y, Yamashita S, Hashimura T, Matsunaga K, Yasuda T. Association between sagittal spinopelvic alignment and femoral head destruction in the early stage of rapidly destructive coxopathy. Bone & Joint Open 2022; 3- 1:77-84.
2016-2018 Japanese Society of Physical Fitness and Sports Medicine Project Research
| Research subject | A study on the relationship between hip rotation and anterior cruciate ligament injury in female athletes |
|---|---|
| Research representative | Tadashi Yasuda |
Published paper
- Yasuda T, Oyanagi K, Nakagaki M, Itoh H. Differential effects of hip rotation range on knee abduction biomechanics during double-legged landing between males and females. The Asian Journal of Kinesiology 2020; 22(4): 34-47.
doctor-initiated clinical trial
| Research subject | Investigator-initiated clinical trial of doctor peripheral blood CD34-positive cell transplantation using MB-001 and IK-02 for patients with intractable fractures (pseudoarthrosis) |
|---|---|
| Research representative | Tadashi Yasuda |
Conference presentation
- Takahiro Niikura, Tomoaki Fukui, Keisuke Oe, Tadashi Yasuda, Goro Tajima, Minoru Doida, Tetsuji Yamamoto, Atsuhiko Kawamoto, Ryosuke Kuroda. Treatment of refractory bone fractures by autologous CD34-positive cell transplantation - report of doctor-initiated clinical trial -. The 21st Annual Meeting of the Japanese Society for Regenerative Medicine, 2022.3.19
2013 Grants-in-Aid for Scientific Research Fundamental Research (B)
| Research subject | Investigation using biomarkers on the effects of exercise therapy on articular cartilage metabolism |
|---|---|
| Research representative | Tadashi Yasuda |
Published paper
- Azukizawa M, Ito H, Hamamoto Y, Fujii T, Morita Y, Okahata A, Tomizawa T, Furu M, Nishitani K, Kuriyama S, Nakamura S, Yoshitomi H, Nakatani T, Tsuboyama T, Hamaguchi M, Matsuda S, Yasuda T The effects of well-rounded exercise program on systemic biomarkers related for cartilage metabolism. Cartilage 2019; 10(4): 451-458.
clinical research
| Research subject | Research representative | Explanatory text (PDF) |
| Retrospective study on paralysis and treatment outcomes of vertebral fractures in diffuse idiopathic hyperostosis (DISH) | Eijiro Ohnishi | |
|---|---|---|
| Observational research for early diagnosis, elucidation of pathology, and establishment of treatment guidelines for rheumatic diseases | Ryohei Saito | |
| Multicenter collaborative research on the treatment of bone and soft tissue infections | Shinnosuke Yamashita | |
| Identification of causative bacteria in pyogenic spondylitis and examination of factors involved in treatment results | Eijiro Ohnishi | |
| Japanese standard treatment with intramedullary nail fixation for tibial shaft fractures: a multi-institutional retrospective cohort study | Shinnosuke Yamashita | |
| Comparative study of in-cage bone fusion between human demineralized bone matrix and autogenous ilium in LLIF | Eijiro Ohnishi | |
| Research on traumatic axillary artery injury | Sadami Mitsuzawa | |
| Research on traumatic popliteal artery injury | Sadami Mitsuzawa | |
| Investigation on treatment results and perioperative complications after cervical spine surgery | Eijiro Ohnishi | |
| Research on factors related to the occurrence of proximal femoral fracture | Tadashi Yasuda | |
| A study on the effect of hip periarticular muscles on femoral neck/trochanteric fracture development | Tadashi Yasuda | |
| A retrospective study on the treatment outcomes of vertebral body compression fractures and burst fractures | Eijiro Ohnishi | |
| Examination of self-injury cases of the wrist joint | Yoshihiro Tsukamoto | |
| Research on factors associated with exacerbation of COVID-19 | Tadashi Yasuda | |
| A large-scale survey of trends and transitions in spine and spinal cord surgery by a multicenter retrospective study | Eijiro Ohnishi | |
| Research on the relationship between humeral diaphyseal fractures associated with pitching and arm wrestling and bone cortex | Tadashi Yasuda | |
| A multicenter observational study using the ``Rheumatology COVID-19 Registry'' | Tadashi Yasuda | |
| A Multicenter Retrospective Study of Lower Lumbar Spine Osteoporotic Compression Fractures | Eijiro Ohnishi | |
| Research on the effects of hip and femoral muscles on functional recovery after total knee arthroplasty and total hip arthroplasty | Yoshi Yasuda | |
| Research on the construction of the The Japanese Orthopaedic Association Case Registry (JOANR) | Yoshi Yasuda | |
| Phase III clinical study of DS-5565 in patients with central neuropathic pain | Yoshi Yasuda | |
| Phase II/III study of MT-5547 in patients with osteoarthritis | Yoshi Yasuda |
Conference presentations/papers
- Yasuda T, Ota S, Mitsuzawa S, Yamashita S, Tsukamoto Y, Takeuchi H, Onishi E. Preoperative lower-limb muscle predictors for gait speed improvement after total hip arthroplasty for patients with osteoarthritis. J. Pers. Med. 2023; 13: 1279.
- Mitsuzawa S, Takeuchi H, Tsukamoto Y, Yamashita S, Ota S, Onishi E, Yasuda T. Risk Factors for the Incidence of the Volar Lunate Facet Fragments in Distal Radius Fractures. J Wrist Surg. 2023; 12(4): 353-358.
- Sadaki Mitsuzawa, Takeharu Nakamata, Shogo Mitamura, Tadashi Yasuda, Shuichi Matsuda. Which head element is more effective for cement augmentation of TFNA? Helical blade versus lag screw. BMC Musculoskeletal Disorders 2023; 24: 544.
- Hashimura T, Onishi E, Ota S, Tsukamoto Y, Yamashita S, Yasuda T. Correction loss following short-segment posterior fixation for traumatic thoracolumbar burst fractures related to endplate and intervertebral disc destruction. BMC Musculoskeletal Disorders 2023; 24: 174.
- Yasuda T, Honda S, Matsunaga K, Hashimura T, Tsukamoto Y, Ota S, Fujita S, Onishi E. Association of preoperative muscle composition of the lower extremity with gait function after total knee arthroplasty. J Orthop Sci. 2023; 28(1) ): 188-194.
- Masuda S, Shimizu T, Sono T, Tamaki Y, Onishi E, Takemoto M, Odate S, Kimura H, Izeki M, Tomizawa T, Tsubouchi N, Fujibayashi S, Otsuki B, Murata K, Matsuda S. Recurrence rate after posterior percutaneous Screw fixation without anterior debridement for pyogenic spondylitis compared with conservative treatment: a propensity score-matched analysis. Eur Spine J. 2023; 32(12): 4265-4271.
- Masuda S, Fujibayashi S, Takemoto M, Ota M, Onishi E, Odate S, Tsutumi R, Izeki M, Kimura H, Tanida S, Otsuki B, Murata K, Shimizu T, Matsuda S. Association of two-staged surgery with systemic perioperative complications in lateral lumbar interbody fusion for adult spinal deformity: a propensity score-weighted study. Eur Spine J. 2023; 32(3): 950-956.
- Hisataka Takeuchi, Kazuaki Morizane, Daisuke Takei, Kazushi Otsuka, Tadashi Yasuda. A rare case of methicillin-resistant Staphylococcus intermedius tenosynovitis. JOS Case Reports 2023; 2(3): 108-111.
- Shinnosuke Yamashita, Sadami Mitsuzawa, Yoshihiro Tsukamoto, Hisataka Takeuchi, Satoshi Ohta, and Tadashi Yasuda. Incidence and clinical characteristics of posterior malleolar fractures associated with tibial shaft spiral fractures. Fractures 45(2)512-515,2023.
- Takataka Azumae, Tetsuhiro Iguchi, Yuo Souda, Keisuke Kinoshita, Takashi Sadamitsu, Hitoshi Yamashita, Kei Kuzuhara, Yoshi Yasuda, Takuhiro Otani, Koichiro Maeno. A survey of the experience and awareness of vertebral fractures due to pregnancy-lactation-related osteoporosis among Orthopedic Surgery surgeons in Hyogo Prefecture. J. Spine Res. 14: 938-944, 2023.
- Sakamoto Y, Onishi E, Hashimura T, Ota S, Takeuchi H, Yasuda Y. Treatment outcomes of lateral lumbar interbody fusion (LIF) for lumbar dialysis-related spondylosis. Journal of the Chubu Japanese Society Orthopedic Surgery Trauma Surgery 2023; 66(1): 61-62.
- Saito, R., Yamashita, S., Ikejiri, N., Takeuchi, H., and Yasuda, Y. A case of comminuted navicular fracture with talonavicular joint dislocation treated with a bridging plate. Journal of the Chubu Japanese Society Orthopedic Surgery Trauma Surgery 2023; 66(5): 751-752.
- Tsukamoto, Y. and Yasuda, Y. A case of traumatic forefoot necrosis requiring soft tissue reconstruction. Orthopaedic and Trauma Surgery 2023; 66(6): 757-761.
- Ryohei Saito, Hiroaki Kimura, Juichi Miura, Bunichiro Wadayama. Two cases in which navigational transverse processectomy was performed for Bertolotti syndrome. Journal of Spine Research 2023; 14(2): 101-106.
- Shinnosuke Yamashita. Plate fixation for femoral condylar and supracondylar fractures. Shin OS NEXUS 7 Lower limb fracture surgery 2: Knee to foot. Edited by Kinshin Watanabe, Medical View, 2023: 2-11
- Yoshi Yasuda. Elucidation of the involvement of Stat3 in joint destruction in rapid-destructive hip disease—Toward clinical application of anti-Stat3 drugs. Kobe City Hospital Bulletin 2023; 62: 62-65.
- Onishi E, Hashimura T, Ota S, Fujita S, Tsukamoto Y, Matsunaga K, Yasuda T. The efficacy and complications of preoperative embolization of metastatic spinal tumors: risk of paralysis after embolization. Spine Surgery and Related Research. 2022; 6(3) ): 288-293.
- Onishi E, Ota S, Fujita S, Tsukamoto Y, Yamashita S, Hashimura T, Matsunaga K, Yasuda T. Association between sagittal spinopelvic alignment and femoral head destruction in the early stage of rapidly destructive coxopathy. Bone & Joint Open 2022; 3( 1): 77-84.
- Honda S, Ota S, Yamashita S, Yasuda T. Inverse association between sarcopenia and displacement in the early phase of fragility fractures of the pelvis. Osteoporosis and Sarcopenia 2022; 8(1); 24-29.
- Yasuda T, Ota S, Yamashita S, Tsukamoto Y, Onishi E. Association of preoperative variables of ipsilateral hip abductor muscles with gait function after total hip arthroplasty: a retrospective study. Arthroplasty 2022; 4: 23.
- Honda S, Fujibayashi S, Shimizu T, Tsubouchi N, Kanba Y, Sono T, Kimura H, Odate S, Onishi E, Tamaki Y, Tomizawa T, Tsutsumi R, Yasura K, Murata K, Otsuki B, Matsuda S. Neurological severity. Evaluation using magnetic resonance imaging in acute spontaneous spinal epidural haematomas. Int Orthop. 2022; 46(10): 2347-2355.
- Yasuda T, Hara S, Yamashita S, Mitsuzawa S, Tsukamoto Y, Takeuchi H, Ota S, Onishi E. Activation of STAT3 (signal transducer and activator of transcription 3) in synovial tissues from the hip joint in the early stage of rapidly destructive coxopathy. Biomedical Research (Tokyo). 2022; 43(5): 173-180.
- Mitsuzawa S, Kusakabe K, Nakao S, Matsuoka T, Yasuda T, Matsuda S. Minimally invasive transiliac anatomical locking plate for posterior pelvic ring injury: a retrospective analysis of clinical outcomes and radiographic parameters for the gull wing plate. BMC Musculoskeletal Disorders 2022; 23: 880.
- Mitsuzawa S, Matsuda S. Cement distribution and initial fixability of trochanteric fixation nail advanced (TFNA) helical blades. Injury 2022; 53: 1184-1189.
- Mitsuzawa S, Kusakabe K, Matsuda S. Minimally invasive transiliac anatomical locking plate for posterior pelvic ring injury: A technical trick of the gull wing plate. J Clin Orthop Trauma. 2022; 33: 101991.
- Odate S, Fujibayashi S, Otsuki B, Shikata J, Tsubouchi N, Tsutsumi R, Ota M, Yusuke K, Kimura H, Onishi E, Tanida S, Ito H, Ishibe T, Matsuda S. Reoperation for misplaced pedicle screws: a multicenter retrospective study. Spine (Phila Pa 1976). 2022; 47(21): 1525-1531.
- Kanta Satsuki, Kentaro Iwata, Kentaro Suzuki, Daisuke Takamura, Yuma Yajima, Akihiro Honda, Nobuo Yukihara, Tadashi Yasuda. Relationship between grip strength before total knee arthroplasty and walking ability 3 months after surgery. Japanese Journal of Artificial Joints 2022; 52: 331-332.
- Kentaro Suzuki, Kentaro Iwata, Kanta Satsuki, Daisuke Takamura, Yuma Yajima, Akihiro Honda, Nobuo Yukihara, Yoshi Yasuda. Effect of limb muscle mass to body weight ratio before total knee arthroplasty on motor function 3 months after surgery. Japanese Journal of Artificial Joints 2022; 52: 335-336.
- Shinnosuke Yamashita, Taku Suzuki, Yuhei Nakayama, Keisuke Ishii, Kento Kurozumi, and Kinnobu Watanabe. Frequency and clinical features of posterior wall-like posterior column fragments in double column fractures. Fracture 2022; 44(1): 48-52.
- Takashi Harada, Satoshi Fujita, Yoshihiro Tsukamoto, Akira Fujita, Tadashi Yasuda. A case of subacute ulnar neuropathy after surgery for a supracondylar fracture of the humerus underwent neurectomy. Chubu Seisai 2022; 65(2): 271-272.
- Satoshi Ota, Shinnosuke Yamashita, Yoshihiro Tsukamoto, Toshifumi Fujita, Eijiro Onishi, Yoshi Yasuda. Efforts to reduce infection in Gustilo classification type IIIB open leg fractures. Edited by Nobuo Adachi. Separate Volume Orthopedic Surgery 81 Treatment strategies for bone and joint infections. Nankodo, Tokyo; 2022: 180-184.
- Tadashi Yasuda, Shigeo Hara, Shinnosuke Yamashita, Sadaki Mitsuzawa, Yoshihiro Tsukamoto, Hisataka Takeuchi, Satoshi Ota, Eijiro Onishi. STAT3 activation in the synovial tissues from the hip joint in the early stage of rapidly destructive coxopathy. The 31st Annual Meeting of the European Orthopaedic Research Society, 2023.9.29, Porto, Portugal
- Yushi Sakamoto, Shinichiro Nakamura, Yugo Morita, Shinichi Kuriyama, Kohei Nishitani, Young Dong Song, Yusuke Yamawaki, Shuichi Matsuda. Tibial Morphology for Proper Adjustment of Metal Augmentation in Revision Total Knee Arthroplasty. ISAKOS 2023, 2023.6.17-21, Boston, USA
- Tadashi Yasuda, Shigeo Hara, Shinnosuke Yamashita, Sadaki Mitsuzawa, Yoshihiro Tsukamoto, Hisataka Takeuchi, Satoshi Ota, Eijiro Onishi. Janus kinase inhibitor can suppress STAT3 activation in the synovial tissues from the hip joint in the early stage of rapidly progressive osteoarthritis of the hip EULAR2023, 2023.5.31-6.3, Milan, Italy
- Ryohei Saito, Takayuki Fujii, Tamami Yoshida, Koichi Murata, Hideo Onizawa, Akira Onishi, Kosaku Murakami, Masao Tanaka, Koichiro Omura, Akio Morinobu, Shuichi Matsuda. Plain hand X-ray-based machine learning model that predicts bone mineral density in RA patients. EULAR2023, 2023.5.31-6.3, Milan, Italy
- Yoshihiro Tsukamoto, Hisataka Takeuchi, Sadami Mitsuzawa, Yoshi Yasuda. Anatomical examination of the lateral femoral circumflex artery system and skin perforators using CT angiography. 50th Annual Meeting of the Japanese Society of Microsurgery, 2023.12.8, Nagoya
- Hisataka Takeuchi, Takayuki Shimoyama, Sadami Mitsuzawa, Yoshihiro Tsukamoto, and Yoshi Yasuda. Recipient vessels around the knee: A study of a lateral crural approach that protects the fibular head: CT image analysis of the anterior tibial artery in the deep posterior compartment. 50th Annual Meeting of the Japanese Society of Microsurgery, December 7, 2023, Nagoya, Japan.
- Ryohei Saito, Eijiro Onishi, Yuji Sakamoto, and Yoshi Yasuda. Correlation between traumatic vertebral fractures and neurological symptoms in patients with diffuse idiopathic osteoarthritis (DISH) and their treatment outcomes. 32nd Annual Meeting of the Japanese Society of Spinal Instrumentation, November 25, 2023, Yonago City
- Shinnosuke Yamashita. Femoral shaft fracture requiring multiple surgeries. Kyoto-Shiga Trauma Conference, 2023.11.25, Kyoto City
- Yuji Sakamoto, Eijiro Onishi, Ryohei Saito, Atsushi Tanaka, Takami Hashimura, and Yoshi Yasuda. Risk factors for failure to identify causative bacteria in pyogenic spondylitis. 32nd Annual Meeting of the Japanese Society of Spinal Instrumentation, November 24, 2023, Yonago City
- Yuji Sakamoto, Eijiro Onishi, and Yoshi Yasuda. Pitfalls in spinal surgery. The 11th Wadachikai, 2023.11.18, Kyoto City
- Nakanishi, Y., Ijiri, K., Sako, D., Shimoyama, T., Furusho, Y., Sakamoto, Y., Segawa, Y., Sakagami, K., Saito, R., Takehara, M., Mitsuzawa, S., Yamashita, S., Tsukamoto, Y., Takeuchi, H., Ohta, S., Onishi, E., and Yasuda, Y. Treatment of distal femoral fractures in elderly patients. The 44th Maya Orthopedic Surgery Hospital-Clinic Collaboration Forum, 2023.11.2, Kobe City
- Hisataka Takeuchi, Sadami Mitsuzawa, Yoshihiro Tsukamoto, and Yoshi Yasuda. Treatment experience with the Outerbridge-Kashiwagi technique for osteoarthritis of the elbow in elderly workers. The 32nd Kyoto Hand Surgery Conference, October 21, 2023, Kyoto, Japan.
- Shinnosuke Yamashita, Kenta Ijiri, Daiki Sakawa, Takayuki Shimoyama, Yuto Nakanishi, Yuya Furusho, Yuji Sakamoto, Yusei Segawa, Koji Sakagami, Ryohei Saito, Genji Takehara, Sadami Mitsuzawa, Yoshihiro Tsukamoto, Hisaki Takeuchi, Satoshi Ota, Eijiro Onishi, Yoshi Yasuda. A case of acetabular bicolumn fracture with posterior wall bone fragments. Hyogo Prefecture Fracture Treatment Study Group, 2023.10.14, Kobe City
- Takehara, M., Mitsuzawa, S., Takeuchi, H., and Yasuda, Y. The rate of greater tuberosity union in reverse total shoulder arthroplasty for shoulder trauma. 50th Annual Meeting of the Japan Shoulder Society, October 13, 2023, Shinjuku-ku, Tokyo.
- Genji Takehara, Tadashi Yasuda, Eijiro Onishi, Satoshi Ota, Hisataka Takeuchi, and Yoshihiro Tsukamoto. A case of total hip arthroplasty for osteoarthritis of the hip in a polio patient. 141st Annual Meeting of the Chubu Japan Orthopedic Surgery Trauma Surgery Society, October 7, 2023, Kobe City.
- Yuji Sakamoto, Eijiro Onishi. Treatment experience and literature review of neck-down syndrome. Spinal Deformity Study Group, 203.9.15, WEB
- Kenta Ijiri, Kenki Ikejiri, Takayuki Shimoyama, Yuto Nakanishi, Yuji Sakamoto, Koji Sakagami, Ryohei Saito, Genji Takehara, Sadami Mitsuzawa, Shinnosuke Yamashita, Yoshihiro Tsukamoto, Hisaki Takeuchi, Satoshi Ota, Eijiro Onishi, Yoshi Yasuda . A case of knee dislocation after revision surgery for supracondylar femoral fracture after TKA. 59th Hyogo Prefecture Knee Joint Study Group, 2023.9.9, Kobe City
- Sadami Mitsuzawa. Dislocated knee fracture with popliteal artery injury. 11th Lower Limb G3C peer review meeting, 2023.9.3, WEB
- Shinnosuke Yamashita. Proximal tibia + diaphyseal fracture case discussion. 7th Kyoto University Orthopedic Residents Meeting, 2023.8.19, WEB
- Koji Sakagami. Fundamentals of tibial shaft fractures. 7th Kyoto University Orthopedic Residents Meeting, 2023.8.19, WEB
- Yuto Nakanishi, Shinnosuke Yamashita, and Yoshi Yasuda. A case of calcaneocuboid joint dislocation fracture. 11th Open Bone Conference Case Study Meeting, August 18, 2023, WEB
- Satoshi Ota, Shinnosuke Yamashita, Yoshi Yasuda. Is trans-iliac rod fixation effective for fragile pelvic ring fractures? 49th Academic Meeting of the Japanese Society for Fracture Treatment, June 30, 2023, Shizuoka City
- Sadami Mitsuzawa, Shinnosuke Yamashita, Yoshihiro Tsukamoto, Hisaki Takeuchi, Satoshi Ota, Eijiro Onishi, Yoshi Yasuda. Five cases of popliteal artery injury associated with trauma around the knee and future treatment plans. 49th Academic Meeting of the Japanese Society for Fracture Treatment, June 29, 2023, Shizuoka City
- Shinnosuke Yamashita, Tadashi Yasuda, Satoshi Ota, Hisataka Takeuchi, Yoshihiro Tsukamoto, and Sadami Mitsuzawa. Anatomical characteristics of the S2 sacroiliac joint screw insertion point and superior gluteal artery in fragility pelvic fractures. 49th Annual Meeting of the Japanese Society of Fracture Therapy, June 29, 2023, Shizuoka City.
- Yoshi Yasuda, Satoshi Ota, Sadami Mitsuzawa, Shinnosuke Yamashita, Yoshihiro Tsukamoto, Hisataka Takeuchi, Eijiro Onishi. Relationship between walking ability after total knee arthroplasty for osteoarthritis and preoperative muscle composition of the affected limb. 60th Annual Meeting of THE JAPANESE ASSOCIATION OF REHABILITATION MEDICINE, June 29, 2023, Fukuoka City
- Noriyuki Ikejiri, Shinnosuke Yamashita, Sadami Mitsuzawa, Yoshihiro Tsukamoto, Hisataka Takeuchi, and Tadashi Yasuda. A case of open fracture of the lower leg with extensive bone defect treated with free latissimus dorsi flap and Masquelet technique. 16th Kyoto University Trauma Research Meeting, 2023.6.3, Osaka, hybrid
- Shinnosuke Yamashita. A case of a fragile pelvic fracture that required hip dissection and fillet flap due to gluteal muscle necrosis and hematoma infection due to superior gluteal artery injury during percutaneous screw insertion. 37th Japanese Society of Traumatology General Meeting/Academic Meeting, 2023.6.1, Nagoya
- Yasuda, Y., Ota, S., Mitsuzawa, S., Yamashita, S., Tsukamoto, Y., Takeuchi, H., and Onishi, E. The relationship between preoperative muscle composition factors of the affected hip abductor muscles and walking function after total hip arthroplasty. 96th Annual Meeting The Japanese Orthopaedic Association, May 12, 2023, Yokohama, Japan.
- Yasuda T. Association of preoperative variables of ipsilateral hip abductor muscles with gait function after total hip arthroplasty. 67th Annual Meeting of Japan College of Rheumatology, 2023.4.26, Fukuoka City
- Ryohei Saito, Takayuki Fujii, Tamami Yoshida, Koichi Murata, Hideo Onizawa, Teru Onishi, Kosaku Murakami, Mao Tanaka, Akio Morinobu, Shuichi Matsuda. Building AI model that predicts change of bone mineral density from plain hand X-ray in RA patients using KURAMA cohort. 67th Annual Meeting of Japan College of Rheumatology, 2023.4.25, Fukuoka City
- Hisaki Takeuchi, Sadami Mitsuzawa, Yoshihiro Tsukamoto, Yoshi Yasuda. Efficacy of triamcinolone acetonide in patients with spring finger under 65 years and over 65 years. 66th Annual Meeting of Japanese Society for Surgery of the Hand(JSSH), 2023.4.21, Shinjuku-ku, Tokyo
- Yuji Sakamoto, Eijiro Onishi, Ryohei Saito, Atsushi Tanaka, Takami Hashimura, and Yoshi Yasuda. Study of the detection method of causative bacteria in pyogenic spondylitis. 52nd Annual Meeting The Japanese Society for Spine Surgery and Related Research, 2023.4.13-16, Sapporo, Japan.
- Yuto Nakanishi, Taiki Sakazaki, Hiroki Konishi. Basics of trochanteric femoral fractures. 6th Kyoto University Orthopedic Residents Meeting, 2023.4.15, Kobe City
- Ryohei Saito, Shunsuke Fujibayashi, Noriaki Shimizu, Koichi Murata, Bungo Otsuki, Shuichi Matsuda. High-level misidentification in spine surgery: A multicenter retrospective study. 52nd Annual Meeting The Japanese Society for Spine Surgery and Related Research, 2023.4.14, Sapporo
- Ryohei Saito, Shinnosuke Yamashita, Kenki Ikejiri, Hisaki Takeuchi, Yoshi Yasuda. A case of comminuted scaphoid fracture with talonavicular joint dislocation treated using a bridging plate. 140th Central Japan Orthopedic Surgery Disaster Surgery Society, 2023.4.7, Nara City
- Yuto Nakanishi, Hiroaki Kimura, Bunichiro Wadayama. A case of thoracic epidural hemangioma with spinal cord symptoms. 140th Central Japan Orthopedic Surgery Disaster Surgery Society, 2023.4.7, Nara City
- Sakamoto, Y., Ohta, S., Ikejiri, N., Saito, R., Sakagami, K., Takehara, M., Wada, A., Kato, R., Tanaka, A., Mitsuzawa, S., Yamashita, S., Tsukamoto, Y., Takeuchi, H., Onishi, E., and Yasuda, Y. A case of primary total knee arthroplasty (TKA) for comminuted fractures of the tibial plateau and proximal tibia. Hyogo Prefecture Fracture Treatment Study Group, April 1, 2023, Kobe City
- Shinnosuke Yamashita. A case of superior gluteal artery injury during trans-sacral screw insertion. Teikyo Trauma Talk, 2023.2.25, WEB
- Shinnosuke Yamashita. A case of tibial plateau fracture: considering initial treatment and final fixation. 15th Kyoto University Trauma Research Meeting, February 11, 2023, WEB
- Hisaki Takeuchi, Sadami Mitsuzawa, Yoshihiro Tsukamoto, Kenki Ikejiri, Yoshi Yasuda. Treatment results of press-fit type artificial radial head. 35th Japanese Elbow Society Academic Meeting, 2023.2.4, Yamagata City
- Yasuda T, Ota S, Yamashita S, Tsukamoto Y, Onishi E. Association of preoperative variables of ipsilateral hip abductor muscles with gait function after total hip arthroplasty: a retrospective study. The 8th Annual Meeting of ASIA, 2022.8.27, WEB
- Yasuda T, Yamashita S, Ota S, Onishi E. Possible association of cortical thickness with spontaneous non-traumatic fracture patterns of the humeral shaft. ECTS2022, 2022.5.7-10, Helsinki, Finland
- Ryohei Saito, Satoshi Ota, and Yoshi Yasuda. A case of osteosynthesis for pelvic fragility fracture, which is difficult to distinguish from pathological fracture. 10th Open Bone Conference Case Review Meeting, 2022.12.10, WEB
- Hisataka Takeuchi, Sadami Mitsuzawa, Yoshihiro Tsukamoto, Ryosuke Ikeguchi, Yoshi Yasuda. Application of the Masquelet method to the treatment of neurological deficits-Study on the usefulness of induced membrane in rat neurodeficient models. The 49th Annual Meeting of the Japanese Society of Microsurgery, 2022.12.1, Hamamatsu
- Yuji Sakamoto, Eijiro Onishi, Takumi Hashimura, Akihiro Wada. Outcomes of lateral route lumbar interbody fusion (LIF) for lumbar dialysis spondylosis. The 31st Annual Meeting of the Japanese Society of Spine Instrumentation, 2022.11.25-26, Osaka
- Kota Wada, Takumi Hashimura, Eijiro Onishi, Itsuro Yamane, and Yuji Sakamoto. Comparison of posterior fusion and anterior-posterior fusion using X-core2 for osteoporotic vertebral body fractures. The 31st Annual Meeting of the Japanese Society of Spine Instrumentation, 2022.11.25, Osaka
- Shinnosuke Yamashita. A case of nonarthrosis of Infra-isthmal fracture of distal femur. 10th Wadokai Case Study Meeting, 2022.11.19, Kurashiki City
- Atsushi Tanaka, Shunsuke Fujibayashi, Bungo Otsuki, Takaaki Shimizu, Koichi Murata, and Shuichi Matsuda. A case of intrathoracic cerebrospinal fluid leakage after anterior thoracic OPLL decompression surgery. The 58th Spine Surgery Study Group, 2022.11.19, WEB
- Yasuda Yoshi. Association between femoral head fracture and sagittal spine-pelvic alignment during the early onset of rapid-destructive hip arthropathy. The 49th Annual Meeting of the Japanese Hip Society, 2022.10.29, Yamagata
- Yuji Sakamoto, Eijiro Onishi, Takumi Hashimura, Satoshi Ohta, Hisataka Takeuchi, Yoshi Yasuda. Outcomes of lateral route lumbar interbody fusion (LIF) for lumbar dialysis spondylosis. The 139th Chubu Japan Orthopedic Surgery Traumatology Society/Academic Meeting, 2022.10.28-29, Osaka
- Atsushi Tanaka, Shunsuke Fujibayashi, Bungo Otsuki, Takaaki Shimizu, Koichi Murata, and Shuichi Matsuda. A case of intrathoracic cerebrospinal fluid leakage after anterior thoracic OPLL decompression surgery. 2nd Kyoto University & University of the Ryukyus & Shinshu University Spinal Osteoporosis WEB Conference, 2022.10.25, WEB
- Tetsuhiro Iguchi, Takaki Higashimuka, Hiroo Souda, Keisuke Kinoshita, Takashi Sadamitsu, Takanobu Azuma, Natsuko Funada, Hitoshi Yamashita, Kei Kuzuhara, Yoshi Yasuda, Takuhiro Otani, and Koichiro Maeno. A survey of experience and awareness of vertebral fractures due to pregnancy/lactation-related osteoporosis among Orthopedic Surgery surgeons in Hyogo Prefecture. The 30th Annual Meeting of the Japanese Society for Low Back Pain, 2022.10.22, Morioka City
- Shinnosuke Yamashita. A case of hip joint dislocation fracture complicated by femoral head fracture. The 35th Hyogo Prefecture Fracture Treatment Study Group, 2022.10.22, Kobe City
- Shinnosuke Yamashita. A case of proximal tibia fracture treated initially in the prone position. OTM Symposium Follow-up small group discussion, 2022.10.20, WEB
- Tadashi Yasuda, Satoshi Ota, Shinnosuke Yamashita, Sadami Mitsuzawa, Yoshihiro Tsukamoto, Hisataka Takeuchi, Eijiro Onishi. Relationship between preoperative factors of affected hip abductor muscles and walking function after total hip arthroplasty. The 74th The Hyogo Prefecture Medical Association Medical Association, 2022.10.16, Kobe City
- Tadashi Yasuda, Satoshi Ota, Shinnosuke Yamashita, Sadami Mitsuzawa, Yoshihiro Tsukamoto, Hisataka Takeuchi, Eijiro Onishi. Dislocation of fragility pelvic ring fracture early onset and association with sarcopenia. The 77th Annual Meeting of the Japanese Society of Physical Fitness and Sports Medicine, 2022.9.22, WEB
- Tadashi Yasuda, Satoshi Ota, Shinnosuke Yamashita, Sadami Mitsuzawa, Yoshihiro Tsukamoto, Hisataka Takeuchi, Eijiro Onishi. Fracture dislocation of the posterior pelvic element and sarcopenia are inversely correlated in early fragility pelvic ring fractures. The 24th Annual Japan Osteoporosis Society, September 2-4, 2022, Osaka
- Takumi Hashimura, Rei Kato, Atsushi Tanaka, Eijiro Onishi, Tadashi Yasuda. Comparison of posterior and anterior-posterior fusion using X-core 2 for osteoporotic vertebral body fractures. The 24th Annual Meeting Japan Osteoporosis Society, September 2-4, 2022, Osaka
- Atsushi Nagata, Shinnosuke Yamashita, Toshifumi Fujita, Satoshi Ohta, Eijiro Onishi, Tadashi Yasuda. A case of open pilon fracture treated with retrograde intramedullary nail combined with Masquelet technique. 9th Open Bone Conference Case Review Meeting, 2022.8.19, WEB
- Satoshi Ota, Shinnosuke Yamashita, Yoshi Yasuda. A case of maternal acetabular fracture. The 48th Annual Meeting of the Japanese Society of Fracture Treatment, June 25, 2022, Yokohama
- Shinnosuke Yamashita, Sadami Mitsuzawa, Yoshihiro Tsukamoto, Hisataka Takeuchi, Satoshi Ota, Yoshi Yasuda. Posterior malleolar fractures associated with spiral fractures of the tibial shaft are often posterolateral oblique fractures with a high joint surface occupation rate. The 48th Annual Meeting of the Japanese Society of Fracture Treatment, June 24, 2022, Yokohama
- Yasuda Yoshi. Relationship between walking ability after total knee arthroplasty for osteoarthritis and preoperative muscle composition of the affected limb. JOSKAS-JOSM 2022, 2022.6.18, Sapporo
- Kenki Ikejiri, Shinnosuke Yamashita, and Hisataka Takeuchi. The 14th Kyoto University Trauma Research Society, 2022.6.4, WEB
- Tadashi Yasuda, Satoshi Ota, Satoshi Fujita, Yoshihiro Tsukamoto, Shinnosuke Yamashita, Takumi Hashimura, Kazuhiro Matsunaga, Eijiro Onishi. Association between sagittal spinopelvic alignment and femoral head destruction in the early stage of rapidly destructive coxopathy. The 95th Annual Meeting of the Japanese Orthopedic Association, May 22, 2022, Kobe, Japan
- Yushi Sakamoto, Shinichiro Nakamura, Shinichi Kuriyama, Ehei Nishitani, Yugo Morita, Shuichi Matsuda. Investigation of the optimal inclination angle of metal augmentation in revision knee arthroplasty. The 95th Annual Meeting The Japanese Orthopaedic Association, 2022.5.22, Kobe City
- Tadashi Yasuda. Association of preoperative muscle composition of the lower extremity with gait function after total knee arthroplasty. The 66th Annual General Assembly and Scientific Meeting of the Japan College of Rheumatology, 2022.4.26, Yokohama, Japan
- Takumi Hashimura, Eijiro Onishi, Toshifumi Fujita, Atsushi Tanaka, Tetsuya Miyamoto, Akihiro Wada, Tadashi Yasuda. Comparative study of in-cage bone fusion between human demineralized bone matrix and autogenous bone in LLIF. The 51st Annual Meeting The Japanese Society for Spine Surgery and Related Research, April 21-23, 2022, Yokohama
- Eijiro Onishi, Takumi Hashimura, Atsushi Tanaka, Yoshi Yasuda. Investigation of the risk factors of sagittal spine-pelvic alignment involved in the onset of rapidly destructive hip arthritis and the crushing of the femoral head in the early onset. The 51st Annual Meeting The Japanese Society for Spine Surgery and Related Research, April 21-23, 2022, Yokohama
- Atsushi Tanaka, Eijiro Onishi, Akihiro Wada, Tetsuya Miyamoto, Takumi Hashimura, Toshifumi Fujita. A study on risk factors for postoperative reintubation in anterior cervical spine fusion. The 51st Annual Meeting The Japanese Society for Spine Surgery and Related Research, April 21-23, 2022, Yokohama
- Ryohei Saito, Hiroaki Kimura, Juichi Miura, and Bunichiro Wadayama. Examination of risk factors for C5 paralysis after cervical posterior fusion surgery. The 51st Annual Meeting The Japanese Society for Spine Surgery and Related Research, April 21-23, 2022, Yokohama
- Sadami Mitsuzawa, Kenji Kusakabe, Shota Nakao, Tetsuya Matsuoka, Ryosuke Ikeguchi, Shuichi Matsuda. A study on risk factors for volar lunate facet fragment development in distal radius fractures. The 65th Annual Meeting Japanese Society for Surgery of the Hand(JSSH), April 14-15, 2022, Fukuoka
- Atsushi Nagata, Shinnosuke Yamashita, Toshifumi Fujita, Satoshi Ohta, Eijiro Onishi, Tadashi Yasuda. A case of open pilon fracture treated with retrograde intramedullary nail combined with Masquelet technique. The 138th Chubu Japan Orthopedic Surgery and Trauma Surgery Society, 4.8-9, Nagoya
- Satoshi Ota. Efforts to reduce infection in open leg fractures. The 34th Hyogo Prefecture Fracture Treatment Study Group, 4.2, Kobe City
- Takahiro Niikura, Tomoaki Fukui, Keisuke Oe, Yoshi Yasuda, Tadashi Yasuda, Goro Tajima, Minoru Doida, Tetsuji Yamamoto, Atsuhiko Kawamoto, Ryosuke Kuroda. Treatment of refractory fractures by autologous CD34-positive cell transplantation - report of doctor-initiated clinical trial -. The 21st Annual Meeting of the Japanese Society for Regenerative Medicine, 3.19, WEB
- Shinnosuke Yamashita. A case of severely comminuted tibial plateau fracture. Teikyo Orthopedic Trauma Talk, 2.26, WEB
- Yoshihiro Yasuda, Kazuhiro Matsunaga, Takumi Hashimura, Shinnosuke Yamashita, Yoshihiro Tsukamoto, Satoshi Ota, Toshifumi Fujita, and Eijiro Onishi. Relationship between walking ability after total knee arthroplasty for osteoarthritis and preoperative muscle composition of the affected limb. The 52nd Annual Meeting of the Japanese Society for Artificial Joints, 2.25, Kyoto
- Satoshi Ohta and Yoshinori Yasuda. A report of one-stage THA using the Harrington technique for elderly acetabular fractures. The 52nd Annual Meeting of the Japanese Society for Artificial Joints, 2.25-26, Kyoto
- Kanta Satsuki, Kentaro Iwata, Kentaro Suzuki, Daisuke Takamura, Yuma Yajima, Nobuo Yukihara, Yoshi Yasuda. Relationship between grip strength before total knee arthroplasty and walking ability 3 months after surgery. The 52nd Annual Meeting of the Japanese Society for Artificial Joints, 2.26, Kyoto
- Kentaro Suzuki, Kentaro Iwata, Kanta Satsuki, Daisuke Takamura, Yuma Yajima, Akihiro Honda, Nobuo Yukihara, Yoshi Yasuda. Effect of limb muscle mass to body weight ratio before total knee arthroplasty on motor function 3 months after surgery. The 52nd Annual Meeting of the Japanese Society for Artificial Joints, 2.26, Kyoto
- Shinnosuke Yamashita, Rei Kato, Atsushi Nagata, Tetsuya Miyamoto, Atsushi Tanaka, Takashi Harada, Kazuhiro Matsunaga, Takumi Hashimura, Yoshihiro Tsukamoto, Satoshi Ohta, Toshifumi Fujita, Eijiro Onishi, Yoshi Yasuda. A case of femoral diaphyseal fracture nonarthrosis. The 13th Kyoto University Trauma Research Society, 2.19, WEB
- Atsushi Tanaka, Yoshi Yasuda, Satoshi Ota, Toshifumi Fujita, Shinnosuke Yamashita, Yoshihiro Tsukamoto. A case of cutting and reinserting the nail and performing BHA for femoral neck base fracture under retrograde femoral nail insertion. The 25th Hyogo Hip Research Society, 2.19, Kobe City
- Yoshihiro Tsukamoto, Yoshi Yasuda, Satoshi Ota, Toshifumi Fujita, and Shinnosuke Yamashita. A case of suppurative hip arthritis requiring hip arthroscopy. The 25th Hyogo Hip Research Society, 2.19, Kobe City
news
The paper ``Association of preoperative variables of ipsilateral hip abductor muscles with gait function after total hip arthroplasty: a retrospective study. Arthroplasty 2022; Contest of Arthroplasty, 2020 The Hyogo Prefecture Medical Association Medical Research Award.
リハビリテーション部と行った共同研究成果を発表した論文「Alterations in deep tissue temperature around the knee after total knee arthroplasty: its association with knee motion recovery in the early phase」が、日本理学療法士学会第10回優秀論文表彰優秀賞を受賞しました。
We have been certified as a specialist training facility by the Japanese Society for Surgery of the Hand(JSSH).
August 2011 lucky day
We have been certified as a Board Certified Surgeon training facility for spine and spinal cord surgeons The Japanese Society for Spine Surgery and Related Research.
Auspicious day of April 2020
In the "Kobe City Municipal Medical Center Orthopedic Surgery Specialized Training Program", our hospital will be the core facility, and the Kobe City Municipal Medical Center Nishi Municipal Hospital and Nishi Kobe Medical Center will be partner facilities. In addition to these three hospitals, the National Hospital Organization Himeji Medical Center, Hyogo Prefecture Amagasaki General Medical Center, Toyooka Public Hospital Association Toyooka Hospital, Social Medical Corporation Shinko Memorial Association Shinko Memorial Hospital, and Kyoto University are joint facilities. join the program.
Our department deals with many acute and chronic diseases including trauma. Each case is jointly handled by a Senior Resident in charge and a doctor in charge of each field, and it is possible to accumulate a wealth of experience.
We are planning to hold a special training program information session on May 28, 2021.
Introduction of 2017 Senior Resident Surgery Surgery Achievements
| spine | Upper limb/hand | Lower extremities | Trauma | rheumatism | sports | Child | tumor | others | |
|---|---|---|---|---|---|---|---|---|---|
| A. | 27 | 10 | 12 | 100 | 0 | 2 | 6 | 0 | 13 |
| B. | 30 | 15 | 60 | 90 | 0 | 0 | 15 | 10 | 0 |
| C. | 22 | 48 | 119 | 150 | 2 | 1 | 24 | 3 | 0 |
Impressions of Senior Resident about Orthopedic Surgery training
Senior Resident A
You can experience multiple injuries unique to tertiary emergency. I also feel that I can grow in a well-balanced manner after experiencing chronic diseases such as artificial joints and spine.
Senior Resident B
I feel that it is a privileged environment to experience many severe cases under the kind guidance of staff members who are well versed in their respective specialties. There are some difficult cases, but I am spending fulfilling days while being blessed with the same period and being encouraged. I actively participate in academic conferences and lectures, and have gained valuable experience. I would like to continue to devote myself to the training and put my feet on the ground.
Senior Resident C
At our hospital, we are able to experience a wide range of cases from the acute stage to the chronic stage under the backup of senior doctors. In particular, there are many complicated cases of trauma regardless of the body part, and I think that there are many cases that are very valuable as training because it is not only a simple procedure, but also training to make a solid preoperative plan. Also, regarding artificial joint surgery, you can be involved in surgery from an early stage, and you can gain experience in implant placement and cement procedures. Postoperative management also needs to be done in a responsible position as the attending physician, and I can feel that I am involved with the patient comprehensively. Therefore, I need to update my knowledge of not only Orthopedic Surgery but also other departments to some extent, which may be a little burdensome, but I think I am in an environment where I can grow as a doctor comprehensively. Senior doctors can equally handle duty and standby duty, so it is possible to devote holidays to your own time, and it is an environment that makes it easy to participate in seminars and academic conferences. I am full of gratitude to Director Yasuda and the other senior medical staff for providing me with training in an environment where I can learn both in classrooms and in practice at a high level.
Senior Resident D
I started my new post in October 2015. The specialized training at our clinic is still short, about 5 months, but I would like to write about two features of the training at our clinic.
The first is the ability to touch various wounds. Since our hospital focuses on emergency care, we will be in charge of various trauma cases. I thought I had experienced all kinds of injuries at the hospitals I worked at, but there were many cases that I had never experienced or that were difficult to treat.
The second is that you can learn about various specialized fields. Various cases have been introduced from Kobe City and surrounding areas. For example, during the 5 months of training, I had the experience of operating about 15 cases of THA. Among them, there are many difficult cases such as CDH and after Chiari surgery, and I am able to accumulate treatment experience that I can use in the future.
What makes this possible is that we have experts in each field who provide guidance and backup. I think it's wonderful to be able to do specialized training in such an environment. It's easy, but I wrote about the characteristics of the specialized training at our clinic.
Recruiting Orthopedic Surgery Senior Resident for 2024
An information session for the Kobe City Medical Center Orthopedic Surgery Specialty Training Program will be held from 6:00 PM on May 10, 2024.
Click here for details