Pelvic Organ Prolapse - Release Your Fear and 6 Ways to Start Healing
Pelvic organ prolapse can feel both frightening and uncomfortable. Maybe you feel like you’re sitting on a small ball, or that something is dragging or falling out of your vagina. You might be experiencing trouble with fully emptying your bladder or bowels when going to the bathroom. Perhaps you are afraid to lift heavy weights, run, or perform your favorite HIIT workouts because you believe that they may worsen your prolapse.
Whether it’s a uterine prolapse, bladder prolapse, or rectal prolapse, this potential diagnosis may have you feeling scared and uncertain of where to turn to for answers.
I see you and I’m here to mitigate your fears as much as possible. A pelvic organ prolapse can feel daunting. But it does not have to be.
First and foremost, you’re not alone. Women, just like you, reach out to me every month with concerns about their prolapse. And many more women find healing and relief from their prolapse symptoms with simple lifestyle changes, and through pelvic floor occupational or physical therapy (when possible).²
I’m eager to share the research behind pelvic organ prolapse, what it is and isn’t, and what steps you can take today to relieve your fears and discomfort.
What is Pelvic Organ Prolapse?
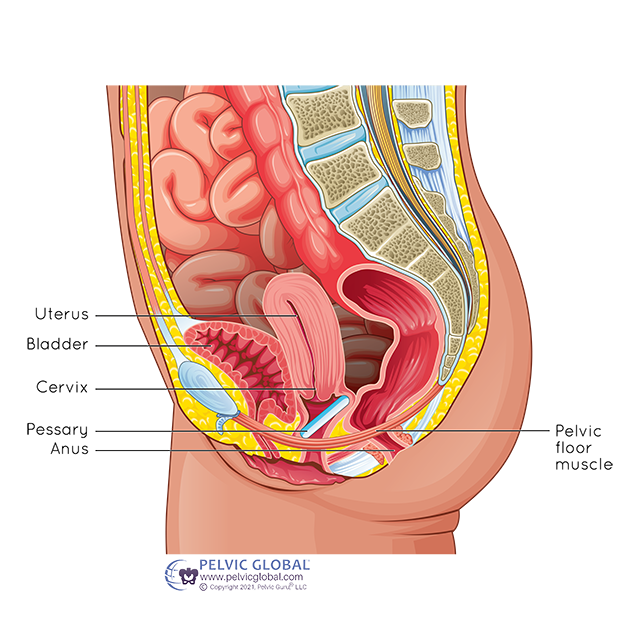
Pelvic organ prolapse is when your pelvic floor muscles, ligaments, and tendons weaken to the point that one or more of the pelvic organs move into the vaginal wall and space. When working properly, the pelvic floor muscles, tendons, and ligaments are strong enough to keep the organs in their proper place. Still, sometimes the pelvic organs may begin to shift downwards because of slow changes over time or specific life events. ³
Pelvic organ prolapse is not as scary as it sounds or may feel! Your organs are not actually falling out. In the case of a rectal or bladder prolapse, your organs move into the space behind the vaginal wall. With a uterine prolapse, your uterus moves into the space of the vagina but is still held up by multiple ligaments. Your ligaments are incredible and almost impossible to break, so even if the pelvic floor changes enough for a uterine prolapse to occur, it is not the same as an organ falling out of your vagina.
Simply put, prolapse is a series of events that add up to an eventual change or shift in the tissues. You’ve done nothing wrong to be where you are. There are common risk factors that can be mitigated – which will be discussed later – but there are also times when our bodies change to the point where we need to compensate and accept the changes.
Nearly 50% of adult women experience some degree of pelvic organ prolapse. This statistic may be even higher because some women don’t report their symptoms to their providers, while others live with varying degrees of pelvic organ prolapse and don’t even know it! ²
The symptoms associated with pelvic organ prolapse often leave women feeling anxious, fearful, and hopeless.
Stages of Pelvic Organ Prolapse
As you might have guessed, there are different stages of prolapse. A proper pelvic organ prolapse diagnosis can be made by a qualified gynecologist, urogynecologist, or nurse midwife.
There are four stages of prolapse, which are graded on the Baden-Walker Scale.
Stage 0: No prolapse
Stage 1: Tissue descends more than 1 cm above the level of the hymen
Stage 2: Tissue is within 1 cm of the hymen (above or below)
Stage 3: Tissue is between 1-2 cm below the hymen
Stage 4: Tissue is more than 2 cm below the hymen
In order to determine which level your prolapse is, it is best to have a vaginal exam while you are laying down and standing because gravity can make a prolapse descend further down. There may also be prolapses that should be diagnosed with ultrasound or imaging as opposed to internal examination.
Risk Factors of Pelvic Organ Prolapse
So what are the causes and risk factors of pelvic organ prolapse? That’s a great question. The leading risk factors for prolapse are:
Having one or more vaginal births
Advanced maternal age with your first baby
Giving birth to a large baby in an un-optimal position
Advanced age
Obesity
Prior pelvic surgery such as a hysterectomy
Chronic constipation
Family history of weak connective tissue or low collagen
Caucasian or Hispanic ethnicity
Chronic coughing
Repeated heavy lifting with improper breathing and form
What do these all have in common? Most of these factors cause increased intra-abdominal pressure which puts a strain on the pelvic floor. But what does that actually mean?
When our pelvic floor muscles are working properly during our daily activities, our pelvic organs are supported up in the pelvis by our pelvic floor muscles. But when we repeatedly cough, hold our breath, become constipated, carry additional body weight, or have a vaginal birth with less-than-optimal breathing, we put an exorbitant amount of stress on our pelvic floor muscles, causing them to become weak.
Think of this analogy: Imagine your pelvic floor is like a trampoline that supports the people (or organs) on it. The trampoline lining should have just enough tension to be able to hold up the people who are bouncing throughout the day; if the lining is too loose, the people may sag down on the trampoline. If the lining is too tight, and the people attempting to bounce may cause damage to the lining. Now imagine that not just one person, but many people are jumping on the trampoline at the same time. Many people jumping puts a lot more strain on the trampoline. The trampoline is like your pelvic floor muscles; when there is too much weight or repeated strong forces placed on a trampoline lining, the lining can stretch and weaken. This is just like your pelvic floor muscles that are supporting your organs in place.
Fortunately, we can take control of our intra-abdominal pressure management and some of these risk factors! There are ways to move our bodies, give birth, and even poop that creates less strain on our pelvic floor and decreases our risk of getting a prolapse or worsening a prolapse.
In addition to preventing or worsening a prolapse, there are also actions we can take to improve the symptoms of prolapse.
Symptoms of Pelvic Organ Prolapse
When considering the symptoms, you first must determine what kind of prolapse you might or might not have.
Something important to note, symptoms don’t always equal severity. One woman may experience multiple symptoms of prolapse and have a very low-grade prolapse. Whereas another woman might not have any symptoms but have a higher-grade prolapse. There are many factors involved in a proper prolapse diagnosis.
Bladder Prolapse
Bladder prolapse, also called a ‘cystocele”, is a prolapse of the anterior vaginal wall. Anterior means the vaginal wall towards the front of your body, where the bladder moves into the vaginal space. Signs and symptoms of bladder prolapse may include:
Pressure or fullness in the pelvis or vagina
A bulge of tissue you can see or feel in your vagina
Increased pelvic pressure when you sneeze, cough, or lift something heavy
Trouble urinating, feeling like you can’t empty completely, or the need to push on the inside wall of your vagina to help the flow
If you are struggling with any of these symptoms, there is hope! Read on for more information on what can be done or email me here with your questions and concerns.
Uterine Prolapse
Uterine prolapse is most common after childbirth or after menopause. Symptoms include:
All the same symptoms as bladder prolapse plus,
Trouble going poop
Problems with leaking urine
Feeling like you’re sitting on a small ball
Pressure or discomfort in your pelvis or lower back
Problems with sex, feeling like something is in the way or the tissue is loose
In the cases of post-childbirth, the grade and symptoms usually improve on their own, but if at any time your symptoms prevent you from normal daily activities, it’s important to seek help. If your symptoms are present long after childbirth or you’ve never had a baby and you have symptoms, it’s important to see your midwife, OBGYN, GYN, urogynecologist, and/or pelvic floor therapist for an evaluation.
Rectal Prolapse
A rectal prolapse also called a ‘rectocele’ is a prolapse of the posterior vaginal wall (back side of the vagina) where the muscles and tissues move and allow the rectal tissues into the vaginal space.
Symptoms can look like this:
Difficult bowel movements
Pressure or fullness in your rectum
A soft bulge of tissue in your vagina
Concerns with your sexual health
Often, rectocele is not the only prolapse present. It would be prudent to assess whether you have other pelvic organ prolapses so you can get the best treatment plan possible.
How to Find Healing from Prolapse…and Start Living Your Life!
Emotional and physical healing from your prolapse is possible; however, it may not look the way you think! While the grade of your prolapse may or may not improve, you can find a great amount of daily symptom relief, guidance, and support through a pelvic floor therapist. A pelvic floor therapist familiar with pelvic organ prolapse can help you to manage your symptoms so you can return to running, lifting, dancing, and picking up your children with decreased symptoms and significantly less fear!
So what can you do to begin managing your symptoms associated with pelvic organ prolapse?
1. Manage Your Intra-Abdominal Pressure
Intra-abdominal pressure is simply the space fully contained between your diaphragm and pelvic floor. How you breathe and move can increase this pressure during your daily tasks. Things like holding your breath, straining, or pounding on the ground, can increase this abdominal pressure and place a great amount of strain on your pelvic floor. The less strain you put on your pelvic floor on a day-to-day basis when you can control it, the better the structures will maintain their strength and integrity, and can support you when you can't consciously control the pressures.
You can manage your intra-abdominal pressure by:
“Blow as you go” – Breathe out when doing certain movements like picking up your child, lifting heavy objects, jumping into a squat, or going up the stairs. All of these put pressure on your pelvic floor. When you breathe out, you constrict your abdomen up and away from your pelvic floor
The knack – Similar to a kegel but not held quite as long, the knack is a well-researched breathing technique that encourages you to squeeze your pelvic floor muscles when you know exertion is coming, such as a sneeze or when you raise your voice. Both of these put more pressure on your pelvic floor so if you can counteract that pressure with a strong pelvic floor, you can reduce unwanted symptoms.
Manage constipation – You want easy and smooth bowel movements at all times. Frequent straining to poop can place a lot of pressure on the pelvic floor, causing the muscles to become overworked and weakened. Making sure you have adequate water and fiber in your diet is key to having easy bowel movements! And if you feel the urge to poop… sit with a flat back, take a deep inhale, and relax so everything comes out slowly and harmoniously. Pro tip – get a stool or squatty potty to prop your feet above your hips! It puts your bowels in an optimal position and makes bowel movements much easier.
2. Pelvic Floor Muscle Training (PFMT)
At the current time of writing, if you go to search engines to learn about how to heal your prolapse, many websites will instruct you to “do Kegels!” However, most people are not aware of how to perform a proper Kegel, and research doesn’t support that this practice actually improves pelvic organ prolapse.
While strengthening pelvic floor muscles definitely has its time and place, Kegels can actually cause more harm if some of the pelvic floor muscles are too “tight” (hypertonic) rather than too “lax” (hypotonic). A shortened, tight muscle can not be adequately moved in order to strengthen it, so needs to be lengthened before it’s strengthened!
While research does indicate that a prolapse grade can at times be improved through strengthening, there are cases where a Kegel does not improve your prolapse.
In general, it is absolutely best to get evaluated by a trained occupational or physical pelvic floor therapist to determine what type of pelvic floor muscle training is best for your specific anatomy, and to seek guidance before starting a pelvic floor exercise routine. ¹
3. Pessaries
Advances in technology have made it possible to create internal devices, called pessaries, to support your muscles. And using a tool like a pessary can be life changing for many women, allowing them to freely exercise and live the life they want with comfort and peace of mind.
A pessary is a small tool that you insert into your vagina to help support your pelvic organs. It can be used for short or long-term therapy and can be a game-changer to help support your muscles.
Think of a pessary like any other support garment. There are over 400 types of pessaries in order to fit each woman as precisely as possible, but they can only be fit by a doctor or trained healthcare professional.
A pessary might be the difference between healing and thriving with a pelvic organ prolapse. Some medical-grade, high quality pessaries can stay in place for weeks, giving you more freedom and flexibility. While being fitted for a medical-grade pessary requires a fitting through a trained healthcare professional (often a gynecologist), there are disposable options that you could try that are available online and over-the-counter to see if a pessary may be a good option for you.
Check out these links for my top recommended over-the-counter trial pessaries!
4. Rest and Elevate
This simple technique is especially important and quite effective to quickly help manage your symptoms. At the end of the day, or whenever you feel your symptoms are most problematic, take some time to lay down and elevate your hips and/or feet; this technique is called “wedging” and allows gravity to assist with bringing your prolapse away from the vaginal canal and gives your pelvic floor musculature a rest. Lay on your back with a wedge or multiple pillows under your pelvis, or even with your legs elevated on a chair or the wall.
Breathe and relax! Our bodies do a lot of work against the force of gravity to keep us in order all day, and honoring rest can do wonders.
5. Practice Mindfulness and Find Your Tribe
Read through Reddit threads, Instagram feeds, and YouTube comments, and you’ll quickly realize you’re not alone. With more than 50% of women having some degree of pelvic organ prolapse, you don’t have to suffer in shame, regret, or fear.
Some of my favorite resources include:
MindYour POP – Lara May is trained pelvic health occupational therapist in Ontario Canada, and provides online courses for those struggling with pelvic organ prolapse so they help utilize mindfulness techniques so you can live in greater freedom.
Postpartum_prolapse – On this great Instagram account, Margo speaks of her experience being a trained athlete and how pelvic organ prolapse changed her life, and how she has found healing.
6. Surgical Repair
If you ever have a provider who immediately recommends surgical repair, I would recommend getting a second opinion. That being said, in rare cases of pelvic organ prolapse, where the prolapse is a more severe grade, surgical repair may be the best option. But pelvic floor therapy and lifestyle changes should almost always be considered first-line treatment prior to and after surgery. Surgery shouldn’t have to be the first and only option!
Find Healing and Freedom From Your Prolapse Symptoms through Calko Pelvic Rehabilitation & Wellness in Canfield, Ohio
You’re taking the first step of many toward freedom. Freedom from fear, freedom from pain, and freedom from feeling broken and out of control.
If you think you may have a prolapse, or you have been told you have a prolapse but you’ve been given little direction towards healing, I’d love to chat with you. You can email me at lauracalko@calkopelvicrehab.com, or you can set up a free phone consultation with me here to discuss your concerns. I’d be happy to listen to your story and see if there is anything I can do to help you find relief and peace.
Research references:
This article was written in collaboration with Cathryn from Honeycomb Holistic Copy - Women’s Health Copywriter. Many thanks to Cathryn for her significant contribution!